Table of Contents
Correctional Investigator’s Message
National Systemic Investigations
Regional Treatment Centres in Crisis: The Erosion of Mental Health Care in Federal Corrections
Falling Through the Cracks: Federally Sentenced Individuals with Cognitive Deficits
Community’s Burden: The Discontinuity of Post-Release Mental Health Services
An Update on Therapeutic Ranges and Intermediate Mental Health Care
Assessing and Addressing Trauma in Federally Sentenced Women
Mental Health Needs and Services for Indigenous Peoples in Federal Corrections
Correctional Investigator’s Outlook for 2025-26
Ed McIsaac Human Rights in Corrections Award
ANNEX A: Summary of Recommendations
Correctional Investigator’s Message
After much reflection, I have decided that this will be my final annual report. I intend to retire at the end of January 2026, concluding 30 years of public service—two years ahead of the end of my current five-year term. This timeline will allow for the public release of my final report in fall 2025 and provide the Government of Canada with sufficient time to appoint a qualified successor to lead the Office of the Correctional Investigator (OCI).
This was not an easy decision. It has been a privilege to serve at the OCI for the past 20 years, including the last nine as Correctional Investigator. As my predecessor, Howard Sapers, often reminded me, this is the dream job for anyone passionate about prison reform and human rights. Leading an independent prison ombudsman office and working with dedicated professionals to ensure that the Correctional Service of Canada (CSC) upholds the rule of law and makes fair, accountable decisions in the administration of federal sentences has been both an extraordinary and fulfilling experience.
I have always been honoured to make evidence-based recommendations aimed at improving conditions of confinement and the treatment of federally incarcerated individuals and those serving the remainder of their federal sentence on conditional release. Speaking truth to power is a responsibility that I have never taken lightly. It is a necessary part of a healthy democracy. It is a challenging yet deeply rewarding role. However, holding the CSC accountable for mismanagement, unfair decisions, and human rights violations has not been without its toll.
I take immense pride in the work my team and I have accomplished in delivering world- class independent prison oversight and ombudsman services. I had the occasion to reflect on these accomplishments recently when our Office celebrated its 50th anniversary in 2023. It inspires a great sense of pride when I consider the cumulative years my team and I have tirelessly spent behind the prison walls and on the phone lines, listening and responding to concerns brought forward to our Office. On a systemic scale, we have conducted important and, in many cases, ground-breaking investigations into issues covering an array of topics and groups – ranging from issues affecting young adults to those who are aging and dying behind bars. Our ten-year update on Spirit Matters, an examination of Indigenous corrections, as well as the Experiences of Incarcerated Black Individuals, in particular, illustrate the value of this Office in tracking progress on important correctional issues over time and serve as a testament to our persistence in holding the CSC accountable to long-standing problems. During my tenure, my Office has boldly raised issues of fairness regarding the impacts of decision- making on the day-to-day lives of incarcerated persons, including the quality of prison food and the rising cost of living. We have also shown leadership in taking on more emerging issues in Canadian corrections, including sexual coercion and violence and the needs and rights of gender diverse prisoners. Our efforts in both investigating and issuing recommendations in these areas, among many others, have been to give a voice to those whose concerns often go unheard or unaddressed, to shine a light on the darkest places of corrections where inequity often finds itself, and importantly, to document accountability, so that these problems, many of which are well-known, can be prevented, curtailed, and resolved.
While we have achieved significant success in resolving individual complaints, many of our recommendations for systemic reform have too often been disregarded or dismissed by the CSC. Over the years, the Department of Public Safety and successive Ministers have also shown a reluctance to compel CSC to act on OCI recommendations, despite acknowledgment of the soundness of our findings. Despite its crucial mandate and a generous annual budget of $3.2 billion supported by 19,000 employees, federal corrections seemingly remains a low priority within the Public Safety portfolio, which also includes border security, policing, and national security. Given the increasingly complex global landscape, I expect that federal corrections will continue to receive limited attention within this broader public safety agenda. This is deeply unfortunate, as CSC is in urgent need of deep structural reform.
Canadians are not well served by a correctional system that is exceptionally costly and well-resourced by international standards, yet persistently fails to deliver on key correctional outcomes—particularly for Indigenous individuals in custody. While it is reassuring to know that the work of my Office has frequently informed court decisions, human rights complaints, class actions, and pre-trial settlements, such litigation could be avoided if CSC and the Government of Canada addressed long-standing issues more proactively. Meaningful reform would not only improve correctional outcomes and prevent human rights violations, but also reduce the financial, social, and human costs associated with litigation and recidivism.
As I approach my 60th birthday in January 2026, I recognize that it is time for new leadership at the OCI—someone with a fresh perspective and renewed energy who may succeed where I have faced obstacles. Although I will deeply miss this work, I look forward to retirement and spending more time with my family, as well as pursuing my passions for travel, sport motorcycling, downhill skiing, and scuba diving.
Knowing that this would be my final report, I chose to highlight an issue that has defined much of my career: access to and the quality of mental health care in federal corrections. My public service career actually began at CSC, where I completed my Ph.D. dissertation in the Psychology of Criminal Conduct with the CSC Research Division. That foundation, combined with early legal work focused on human rights in Corrections, has shaped my professional path and sustained my focus on the critical importance of mental health services for incarcerated individuals.
This year’s annual report therefore consists of findings from six national investigations into this very issue of access to and quality of mental health care for federally sentenced individuals, including the following areas:
- The overall purpose and functioning of CSC’s Regional Treatment Centres (RTCs).
- Approaches to identifying and addressing the needs of individuals with cognitive deficits.
- Community discharge planning and the continuity of services for individuals with significant mental health issues.
- An update on Therapeutic Ranges and Intermediate Mental Health Care in federal prisons.
- Assessment and treatment of trauma for federally sentenced women.
- Culturally- and trauma-informed mental health and wellness services for Indigenous peoples in federal corrections.
For these investigations, the OCI conducted a grand total of 425 interviews with federally sentenced individuals, both in custody and on community release. We also conducted site visits and met with institutional and community staff, a variety of community-based stakeholders, Indigenous organizations, and provincial correctional authorities, among others. Furthermore, this year’s investigations were strengthened by partnerships and external expertise, including the Office of the Federal Ombudsperson for Victims of Crime and the Centre for Addiction and Mental Health, to support our Office’s investigations into trauma-informed services for women and services for individuals with cognitive deficits, respectively.
There is no question that lack of access to timely, adequate, and appropriate mental health care is a human rights issue. After visiting all five RTCs, four of which are designated psychiatric hospitals, it is abundantly clear that CSC is fundamentally ill-equipped to provide long-term mental health care to individuals with serious mental illness—those experiencing acute psychiatric distress, suicidal ideation, and chronic self-injury.
The findings presented in this report reaffirm our long-standing position: CSC should not be in the business of delivering specialized long-term acute psychiatric care. In cases involving such serious mental illness, transfers to external, secure, community- based psychiatric hospitals are necessary. Consider this analogy: CSC routinely transfers individuals requiring complex physical care—such as chemotherapy or heart surgery—to external hospitals. It would be unthinkable to attempt such procedures in-house. Yet, when it comes to mental health, CSC continues to operate under the misguided belief that it can provide specialized psychiatric care internally.
Our latest findings underscore that RTCs can be best described as intermediate and geriatric care facilities, with limited emergency mental health capacity for acute cases. They should therefore be reprofiled and recognized as such. Individuals with acute and long-term psychiatric complex needs should be transferred, under section 29 of the Corrections and Conditional Release Act (CCRA), to specialized, external facilities capable of delivering the appropriate level and quality of care. Continuing to house these individuals in CSC-operated RTCs is not only ineffective and inappropriate—it is a clear violation of human rights and inconsistent with the United Nations Standard Minimum Rules for the Treatment of Prisoners (the Nelson Mandela Rules) 1 .
Despite decades of investment, CSC remains unable to meet the complex mental health needs of this population. The announcement of a $1.3 billion replacement facility for RTC Atlantic (Shepody) is, in our view, a profound misallocation of resources. Rather than investing in another CSC in-house facility, the Government of Canada should have directed CSC to partner with provincial health systems to expand access to secure psychiatric beds in the community. The CSC could have funded enhanced bed capacity through provincial partnerships—an approach that would be more humane, cost-effective, and sustainable over the long term. The $1.3 billion allocated could cover the costs of such a model for decades to come.2 I urge the Government to reconsider its plans. The CSC is mandated to deliver correctional services, as well as health care services, which includes mental health care; however, they should not be engaged in the provision of acute psychiatric care. Similarly, the federal government should not assume responsibility for such specialized health care services. Instead, it should collaborate and coordinate with provincial health authorities to ensure that federally incarcerated individuals receive timely and appropriate mental health care in settings equipped to provide such care. Ironically, the CSC and the Government of Canada did not consult my Office on their intended investments. Consequently, absent from the plan was the most appropriate option to reform the delivery of acute mental health care and services in federal corrections: the transfer of seriously mentally ill patients to external, provincial psychiatric hospitals. This does not even appear to have been considered, despite being the option advocated not only by my Office, but by the Standing Senate Committee on Human Rights in its 2021 report entitled: Human Rights of Federally-Sentenced Persons. Even Bill S-230: Providing Alternatives to Isolation and Ensuring Oversight and Remedies in the Correctional System Act (Tona’s Law), promotes the approach of transferring individuals with disabling mental health issues to an external hospital.
The lack of transparency and failure to consult more broadly is indicative of how the CSC continues to prioritize what is best for the Service, and not what is best for those in their custody or supervision. The current plan is in violation of the Nelson Mandela Rules and only partnerships with provincial health care facilities will ensure proper care. The seriously mentally ill are patients first, and not inmates first. CSC’s approach has been the latter.
- I recommend that CSC’s RTCs be redefined and formally recognized as Intermediate Mental Health Care facilities, with limited capacity to manage emergency psychiatric cases. Individuals diagnosed with serious mental illness— those experiencing acute psychiatric crises, persistent suicidal ideation, or chronic self-harming behaviours requiring long-term psychiatric care—should be transferred to community-based psychiatric hospitals better suited to meet their needs.
- I recommend that CSC’s RTCs be redefined and formally recognized as Intermediate Mental Health Care facilities, with limited capacity to manage emergency psychiatric cases. Individuals diagnosed with serious mental illness— those experiencing acute psychiatric crises, persistent suicidal ideation, or chronic self-harming behaviours requiring long-term psychiatric care—should be transferred to community-based psychiatric hospitals better suited to meet their needs.
This year’s investigation into cognitive deficits is leading-edge in corrections, not only domestically but internationally, as it is an area that has been neglected. This investigation revealed that given such neglect, the prevalence of cognitive deficits is arguably unknown and likely underestimated. The consequences of such can be seen in the largely absent or ineffective approaches to screening, assessment, programming, and training for staff in relation to working with individuals with cognitive deficits. Vague and ill-fitting policies that do not adequately guide practice or match local realities or needs have consequentially led to stigma, safety issues, and challenges to daily living for those living with cognitive deficits in prison. These gaps and challenges place significant burdens on staff to seek creative solutions and opportunities to up-skill themselves, in some cases at their own expense, in order to meet these pressures and demands.
Also new ground for our Office, our investigation into trauma revealed that, despite nearly all incarcerated women having experienced some form of trauma in their lives, little is done in the way of screening and assessment, and few dedicated resources – particularly psychological supports – to help address the underlying causes of trauma- based responses. As was found in the other investigations, staff shared that they are inadequately prepared to effectively and safely work with women on the root causes of trauma. Relatedly, for Indigenous peoples serving federal sentences, trauma- and culturally-informed mental health and wellness services were found to be severely lacking, despite the significant needs of this population and their well-documented over-representation in the system. As this Office has called for previously and repeatedly, a broader decolonization of the prison system and a transfer of care to Indigenous, community-based organizations and individuals, is what is needed to make meaningful and lasting change.
Disappointingly, our look at progress made since our last reporting on Therapeutic Ranges, as well as the state-of-affairs in intermediate mental health care more broadly, revealed that many of the issues previously raised by this Office and the Service itself, remain and progress has seemingly stagnated. Our investigation into continuity of care and community discharge planning for individuals with serious mental health issues confirmed a similar, long-standing issue – the priority continues to be the resourcing of mainstream, custodial corrections, which has resulted in increased barriers and an overall erosion of mental health resources for those working in, and those being released to, the community.
While each investigation yielded subject-specific findings, given the unifying theme of mental health that runs through all six investigations, some cross-cutting findings and concerns also emerged, including:
- Weak, vague, outdated, and/or absent national policies have led to ineffective, confusing, and inconsistent direction and implementation of mental health services on the ground.
- Insufficient training provided to staff on how to work effectively and humanely with individuals with mental health issues (including those with cognitive deficits, age-related mental health issues, and/or trauma), has contributed to poor responsivity and quality of care in corrections.
- An absence of effective screening and assessment of mental health issues has created a domino effect of poor identification and access to services, thus excluding many who need such enhanced forms of care.
- Adapted and/or specialized options for programming, treatment, or opportunities for skill acquisition that would support preparations for successful release are inconsistent or unavailable.
- Prioritization of security measures, responses (including the use of force), and physical structures prevails over more dynamic, human-centred, and therapeutic forms of interaction and provision of care with individuals with mental health concerns, creating a fundamental conflict between health care and security staff, as well as between patients and staff.
Taken together, this report offers a comprehensive overview of the challenges CSC faces in delivering mental health care. Despite the criticisms contained herein, I wish to acknowledge the commitment and professionalism of CSC’s health care professionals and front-line staff, who do their best under extremely difficult conditions. During the course of our investigations, they provided invaluable and candid feedback.
Finally, I look forward to receiving CSC’s responses to my recommendations in a proper and transparent format, consistent with commitments made by two former Ministers of Public Safety. As the OCI has advocated for two decades, CSC’s responses should clearly indicate whether it agrees, agrees in part, or does not agree with each recommendation. Responses should be concise and should outline concrete actions to be taken, along with specific timelines. This would allow for the integration of CSC’s responses directly beneath each recommendation in the body of the report, as is standard practice across jurisdictions for ombudsman reports. This will also enable our Office to better track progress on an annual basis as well as formally report on responses to our recommendations as a departmental results indicator.
I acknowledge that CSC has not always had the authority to respond directly to some recommendations—for example, those requiring new legislation or additional funding. However, such cases are rare, and this report does not include any recommendations of that nature. In my professional opinion, CSC has the resources and the legislative authority, under the CCRA, to implement all of the recommendations contained in this year’s report. While some reallocation of existing resources may require support or approval from central agencies, I believe such prerequisites can be stated in CSC responses.
Ivan Zinger, J.D., Ph.D.
Correctional Investigator
June 2025
Responses to Recommendations
To ensure clarity, transparency, and accountability, responses to the Office of the Correctional Investigator’s recommendations are embedded throughout this report. Each recommendation is followed by the agency or department’s selected response option and a supporting narrative outlining intended actions and timelines. The response options are defined as follows:
Accepted: The recommendation is fully agreed with and will be implemented as stated.
Accepted in-part: The recommendation is partially agreed with; some elements will be implemented while others will not.
Accepted in-principle: There is agreement with the overall recommendation and underlying conclusions; however, further action is required before the agency can commit to implementation (e.g., conducting consultation, securing new funding). This is therefore a conditional acceptance, acknowledging that further discussion and follow-up with the OCI is necessary.
Rejected: The recommendation is not agreed with and will not be implemented
- I recommend that CSC’s RTCs be redefined and formally recognized as intermediate mental health care facilities, with limited capacity to manage emergency psychiatric cases. Individuals diagnosed with serious mental illness—those experiencing acute psychiatric crises, persistent suicidal ideation, or chronic self-harming behaviours requiring long-term psychiatric care—should be transferred to community-based psychiatric hospitals better suited to meet their needs.
CSC's Response: REJECTED
The Correctional Service of Canada (CSC) acknowledges the need to ensure that inmates have access to the required health care services. and CSC currently has a health system and service delivery model to provide services that are matched to level of need.
To address the health needs of the inmate population, CSC Regional Treatment Centres (RTCs) provide a range of services at both the psychiatric in-patient and intermediate mental health levels of care. Psychiatric in-patient hospital care is provided to inmates who have serious mental health needs and require a hospital environment that provides access to 24-hour health care. Intermediate Mental Health Care is provided to inmates whose needs exceed the level of care provided through primary care at mainstream CSC institutions, based on an assessment of the inmate’s impairment in level of functioning.
Depending on the specific needs identified and level of treatment required, intermediate mental health care services are provided in select CSC institutions, or in RTCs. Currently, a significant proportion of RTC services are targeted to the provision of intermediate mental health care. CSC’s health services, including the RTCs, are accredited by Accreditation Canada, which is the same organization that accredits hospitals and other service providers in communities across the country.
To supplement CSC’s internal in-patient psychiatric capacity, CSC currently has a partnership with the lnstitut Philippe-Pinel de Montréal for the provision of in patient psychiatric care to men and women offenders, subject to meeting Pinel’s admission criteria. CSC will continue to engage with additional provincial psychiatric hospitals to supplement existing capacity for the provision of in patient psychiatric care. This engagement is done in acknowledgement of the limited capacity of provincial health care facilities to provide care to federal inmates, particularly in relation to their ability to admit federal inmates with complex mental health and security needs.
Despite this continued focus on engagement, to ensure that CSC has the capacity to meet its legislative mandate to provide essential health services to inmates, CSC must maintain a critical capacity to provide in-patient psychiatric care in RTCs. CSC is currently conducting a comprehensive review of its RTCs to provide a standardized baseline of service provision. This review will include a focus on ensuring that services provided align with CSC population health needs and reflect an appropriate mix of Psychiatric Hospital Care, Intermediate Mental Health Care, and short-term medical care.
Next Steps: CSC has initiated a review of Regional Treatment Centres to provide a standardized baseline of service provision.
Timeline: Fiscal year 2026-27
- I recommend that the Government of Canada/Minister of Public Safety reconsider its recent $1.3 billion investment in a replacement facility for RTC Atlantic (Shepody). Instead, efforts and funding should be redirected to support CSC in reallocating its current resources toward facilitating the transfer of individuals with serious mental illness to provincial psychiatric hospitals. This includes supporting the creation or expansion of bed space in provinces facing capacity constraints.
Public Safety's Response: REJECTED
The Health Centre of Excellence (HCoE) in Dorchester, New Brunswick, will be a modern, bilingual, purpose-built health care facility that will support CSC in advancing its patientcentered health care model and will set the standard for health care in federal corrections. It will increase bed capacity to better meet the health needs of an increasingly diverse and complex inmate population at both the in-patient and intermediate mental health levels of care. It will also support the provision of care to unique segments of the inmate population including those who have mobility issues; those requiring access to 24-hour care; women; and the Older Persons in Custody (OPIC) population. This facility is necessary in order to address the needs of inmates with mental health issues in the near and long term.
CSC engages with external hospitals to negotiate partnerships to enhance CSC’s capacity to treat individuals with more complex mental health needs. Admissions to external health care facilities are based on a standardized referral process, initiated by CSC, to address specific clinical needs. They are voluntary and require informed consent. It is important to note that CSC cannot compel external hospitals to enter into partnerships with CSC.
In 2024, CSC committed to engaging with forensic psychiatric hospitals to explore opportunities to establish Memorandums of Understanding (MOUs) for mental health assessment, treatment and inpatient care for CSC’s inmate patients. Health Services reached out to 11 external hospitals and all but one declined entering into a partnership for the provision of external psychiatric beds at that time. One external hospital indicated they would be open to future discussions around entering into such a partnership.
That said, the development of the HCoE is not being pursued to the exclusion of CSC’s ongoing partnership engagement. CSC Health Services continues to focus on partnerships in several key areas: access to community hospital beds, including forensic psychiatric beds; external health care services to meet specific health care needs; and specialized care for vulnerable subgroups (e.g., care for older inmates, care to gender diverse inmates).
CSC will continue to ensure that the highest standard of care, in line with community standards, is provided to individuals under CSC’s care.
Executive Director’s Message
It is with deep gratitude and optimism that I step into the role of Executive Director at the Office of the Correctional Investigator of Canada. I am honoured to join a team of dedicated professionals who work tirelessly to uphold fairness and humane treatment in the federal correctional system.
I extend my heartfelt thanks to our outgoing Executive Director, Monette Maillet, for her exceptional leadership. Her contributions have left a lasting legacy—from stabilizing the workforce, to modernizing systems and reducing backlog, to guiding the Office toward compliance with international standards and strengthening our ability to respond to the needs of those we serve. Her leadership has had a lasting and meaningful impact on this Office.
As a human rights lawyer, I have spent my career advancing reconciliation, justice, equity, and accountability. My experience has taught me that public safety and human rights are not at odds, they are in fact deeply interconnected. I am excited to work alongside this incredible team, bringing our shared knowledge and diverse experiences together to strengthen our efforts and ensure that individuals serving federal sentences are treated with dignity, fairness, and humanity. I am proud to highlight some of their achievements.
Over the past year, our Office received 4,352 complaints from federally sentenced individuals—each one representing a voice that deserves to be heard and a concern that matters. We spent more than 96,000 minutes on the phone lines and 433 days inside correctional facilities—efforts that reflect the compassion and dedication of our team, and the importance of being present, listening, and responding in meaningful ways.
In response to the evolving needs of those we serve, the Office has made important strides this year. Using the Lean method, we improved the efficiency of our early resolution and operational processes, allowing us to respond more quickly and effectively. The Office has developed dedicated investigative teams that prioritize tandem institutional visits to ensure consistency and enhanced oversight, with a goal of developing specialized knowledge, strong collaboration, and higher quality operational outcomes. Finally, we introduced a triage process for use of force cases to streamline workflow and prioritize the most urgent and critical reviews with efficient resource allocation.
The Office has expanded our engagement both domestically and internationally sharing best practices, learning from others, and building relationships that help enhance correctional oversight around the world. Our work with Indigenous rightsholders and organizations has been especially important, guiding the ongoing development of a dedicated Indigenous Strategy that reflects our deep commitment to reconciliation and to addressing the systemic inequities faced by Indigenous people in federal custody. We have participated in key conversations at parliamentary committees and conferences, contributing to critical discussions that shape Canada’s criminal justice policies and influence how the rights of incarcerated individuals are protected.
When I first joined the OCI, I met with each employee to get their perspectives on what was going well in the office and where we needed to improve. I was grateful to receive open, honest, and thoughtful feedback.
At a very high level what I heard was that our employees appreciated the trust the office has in them to effectively do their work. They also appreciate the flexibility and understanding given to employees by their managers. The mandate of the organization is a critical one that gives them a sense of purpose. Many feel that there is good collegiality on the team and that they can have open and honest conversations with each other and with management. Employees also appreciate management having an open-door policy.
Some of the challenges I heard included that the volume and challenging content of the work has put some positions at higher risk of burn out. In addition, as this is a micro agency, opportunities for promotion are limited and employees felt that too little attention was invested in their growth and career progression. I also heard there is a need for better internal communication, consistent onboarding practices, job-specific training, and more open competition for jobs. It became clear that this has been a time of significant transition for the organization which saw a turnover in 50% of the executive team, either through retirements or departures. In addition, the Correctional Investigator shared his intention to retire within the next fiscal year. Our employees, like others in the public service, have increased their presence in the office while consideration has been given to their travel, time spent in institutions, and accommodation needs.
The Public Service Employee Survey (PSES) from 2024 echoes this feedback. This is feedback we take very seriously. After briefing the Correctional Investigator, we agreed that we will seek an external resource to support the organization in comprehensively addressing the concerns raised both in my interviews and through the PSES. This will ensure that we have a sound action plan with reasonable timeframes to effect organizational change prior to the departure of the current Correctional Investigator.
Since fully assuming the role of Executive Director in mid-January 2025, the Correctional Investigator, the management team, and I have initiated several changes in response to what we have heard. Performance agreements have been completed for the team and four advertised selection processes were launched. At least two of these processes included external board members as well as external human resources advice. We have begun the creation of a consolidated procedures manual to ensure that all operational staff have access to up-to-date comprehensive information that will support them in their work. The Corporate team is now fully staffed, and we have launched an exercise to renew our human resources policies. New employees are working in teams or are being paired with a “buddy” to ensure they have a dedicated resource to support them in addition to their manager and other colleagues. We are continuing to authorize two investigators to travel to institutions together as frequently as possible in compliance with international standards, but also to support their wellbeing given the challenging work that they do. In addition, we will be launching an Inclusion, Diversity, Equity, and Accessibility (IDEA) committee in the coming months as well as a self-declaration campaign. We will work with a consultant to help develop an Information Management Architecture, which will pave the way to a new document management system to help address a number of irritants in how we organize, store, and access all of our documents. We have also staffed a dedicated Communications position to improve both our internal and external communications with staff and stakeholders, as well as support more proactive and consistent outreach and engagement.
The OCI remains committed to making this a great workplace with concrete action in a reasonable time.
As we prepare for a leadership transition in the year ahead, I want to extend my sincere congratulations to Dr. Ivan Zinger on his exceptional career with the OCI and the federal public service. I look forward to continuing to work with him and learn from him during this time of change and growth. This moment presents a valuable opportunity to reflect, renew, and build on the strong foundation that has been laid, as we refine our investigative, policy, and research work and continue to move our mandate forward.
I’m grateful for the opportunity to build on our collective strengths and to help shape a more humane, accountable correctional system.
None of this progress would be possible without the incredible work of our team. Whether in corporate services, early resolution, operations, policy and research, our specialized portfolios, or our use of force review team—every individual here plays a vital role. Your knowledge, your integrity, and your commitment are what give this Office its strength.
Valerie Phillips
Executive Director
National Systemic Investigations
Regional Treatment Centres in Crisis: The Erosion of Mental Health Care in Federal Corrections
In the Office’s 2023-24 Annual Report, we examined the circumstances that led to the tragic death of Mr. Stéphane Bissonnette, a 39-year-old man who, in December 2021, died in an observation cell while on modified suicide watch at the Regional Treatment Centre (RTC) Millhaven. In addition to spending significant lengths of his sentence in administrative segregation in maximum-security facilities, Mr. Bissonnette had also been subject to various placements in Regional Treatment Centres across the country.
The investigation into Mr. Bissonnette’s death revealed a significant degree of dysfunction at RTC Millhaven including structural, operational, and policy deficiencies. The Office identified a multitude of systemic issues related to his time at multiple RTCs, the events leading to his death, the National Board of Investigation (NBOI) which was subsequently convened, and the findings stemming from the NBOI itself. The need to comprehensively examine the functioning of these facilities on a broader, more systemic level was apparent.
Background
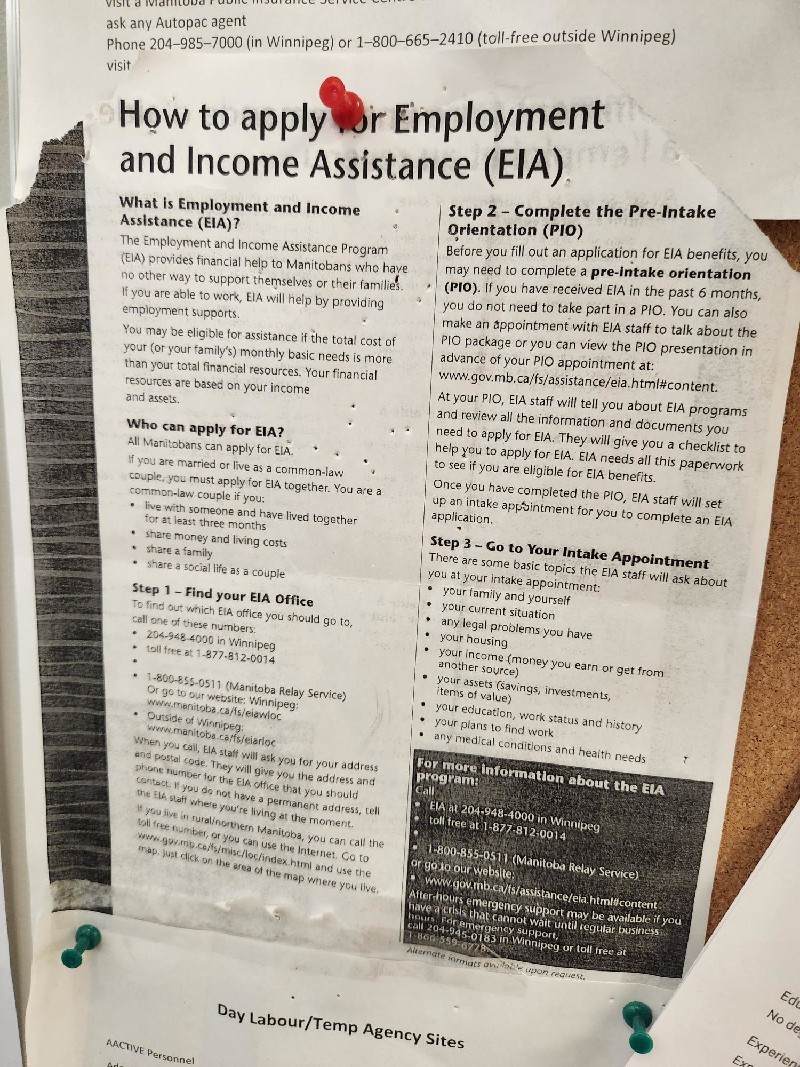
Under the Correctional and Conditional Release Act (CCRA), CSC is required to provide federally sentenced individuals with essential health care and reasonable access to non- essential health and mental health care that will contribute to the individual’s rehabilitation and successful reintegration into the community. When care is provided, the CCRA stipulates that the Service shall promote decision-making that is based on the appropriate medical, dental, and mental health care criteria. In efforts to meet this obligation, CSC operates five Regional Treatment Centres (RTCs) across Canada that provide clinical assessment and inpatient treatment for federally sentenced individuals with serious acute and/or chronic mental health conditions. The primary role of RTCs is to provide specialized services of a “time-limited nature” to stabilize individuals with the expectation that patients, where appropriate, will transition back to their ‘parent’ institution with a plan for continuity of care.
Treatment centres present a unique dynamic in that they are ‘hybrid’ facilities – psychiatric hospitals guided in part by provincial health legislation, operating within a federal penitentiary setting subject to the CCRA. All treatment centres, except for the Regional Psychiatric Centre (RPC) in the Prairie region, are co-located within larger penitentiary sites. Some of these facilities are subsumed within existing penitentiaries, while other treatment centres are found in repurposed or converted buildings.
Table 1. List of Regional Treatment Centres (RTCs) with Rated Bed Capacities and Snapshot of Actual Counts (2024)
| RTC and Location | Co-located Institution | Rated Capacity | Actual Count |
|---|---|---|---|
|
RTC Ontario which includes:
RTC Bath RTC Millhaven |
Bath Institution Millhaven Institution |
36 90 |
36 89 |
| RTC Pacific (Abbotsford, BC) | Pacific Institution | 168 | 129 |
| Regional Psychiatric Centre (Saskatoon, SK) | N/A – Standalone Facility |
184 men /
20 women |
145 men /
9 women |
| Regional Mental Health Centre (Sainte-Anne-des-Plaines, QC) | Archambault Institution | 119 | 83 |
| Shepody Healing Centre (Dorchester, NB) | Dorchester Institution | 38 | 42 |
| Total |
635 men /
20 women |
524 men /
9 women |
Source. Retrieved from the Corporate Reporting System Modernized (CRS-M) on July 11, 2024. 3
In addition to these facilities, the Institut national de psychiatrie légale Philippe-Pinel (INPLPP) in Montréal, Quebec, has five CSC funded beds for men and 15 beds for women, bringing the total capacity to 640 beds and 35 beds, for men and women respectively. As will be discussed later in this section, many of these beds are occupied by geriatric patients or individuals with disabilities and those requiring intermediate care, who may not meet CSC’s criteria for a psychiatric bed.
Nominally, the RTCs fall under CSC’s Health Services Sector, and are headed by an Executive Director. In practice, the Executive Directors work closely with and are accountable to the Warden (at co-located sites), as well as Health Services (at the Regional and National levels), resulting in a confusing organizational structure. In policy, the RTCs are classified as multi-level security facilities, meaning that patients assigned an Offender Security Level (OSL) consistent with minimum, medium, or maximum security can all be housed in the same facility. According to Commissioner’s Directive (CD) 706 - Classification of Institutions, RTC security measures should be dependent on the individual’s classification while the patient’s time at RTC should reflect their security level and be in compliance with their correctional and treatment plans.
Designation as Psychiatric Facilities
All but one of the RTC units are “designated” psychiatric facilities. While specific definitions may vary, designation refers to the formal recognition of a facility as a psychiatric or mental health centre by the provincial government where the RTC is located. In some provinces, the Minister of Health holds the legislative authority to designate psychiatric or mental health facilities while the required services for designation can vary by province as well (e.g., one or more of the following services may be needed to qualify: registered psychiatric nursing, emergency stabilization, observation, rehabilitation services, inpatient or outpatient care, etc.). This variation in requirements raises concerns about consistency in mental health care quality across provinces, as some jurisdictions may have higher service expectations. An outlier, the Regional Mental Health Centre (RMHC) at Archambault Institution is not designated as a “hospital” under provincial legislation due to its legislative framework, a notable difference that highlights potential legal and administrative gaps that affect the relation between federal institutions and provincial mental health care systems.
While CSC could not provide an exact date when individual RTCs were designated in accordance with their respective provincial legislation, it was suggested that this occurred in response to the enactment of the Canada Health Act (1984), which ensured all eligible residents of Canada had access to insured health services without financial or other barriers, and under which federally sentenced individuals were determined to be ineligible. The Penitentiary Act, which previously covered health service delivery for prisoners, was replaced with the enactment of the CCRA in 1992, leading to an effort by the Service to keep parity with community standards and a new focus on centralized health and mental health services.
When seeking designation for a particular facility, CSC must generally apply to the respective provincial ministry of health. Individual ministries may look at elements such as infrastructure, staffing models, location, and how care is delivered. The application process is ordinarily conducted by the Regional Director, Health Services (RDHS) for each region and signed off by the Commissioner.
Notably, once a province designates a particular facility, there are no further evaluations or ongoing mechanisms to ensure adequate services are being provided to maintain designation. Treatment Centres do not have to re-apply to maintain their designation and will, in virtually all cases, maintain this until such time as a facility needs to physically move. For example, following the closure of the treatment centre found within Kingston Penitentiary, a designated Schedule 1 facility 4, and the subsequent displacement of patients until their eventual transfer to Bath and Millhaven Institutions (RTC ON), reapplication to the Ontario Ministry of Health was required. CSC staff advised that, as a result, accreditation is the mechanism most often relied upon to measure adherence to health standards within these facilities. Even in the case of tribunals such as the Consent Capacity Board in Ontario, for example, ruling against the certification of patients to receive care against their will, designation of individual facilities is not called into question.
Designation aside, the health services provided by CSC, including mental health care, are subject to accreditation by Accreditation Canada, an independent non-profit organization responsible for ensuring that these services meet certain standards of quality and safety. These standards, created in consultation with a diverse range of representatives, are developed by the Health Standards Organization (HSO), also a non-profit entity, and form the foundation for the accreditation process. CSC has commissioned the HSO to develop a National Standard of Canada for correctional institutions, which has been subsequently integrated into its accreditation program. According to HSO, the new standard, HSO 34008:2018 (E) Correctional Services of Canada Health Services, is specifically designed to address the needs of federal correctional institutions, recognizing the link between the wellbeing of incarcerated individuals and their human rights (HSO, 2024). 5
Generally, meeting accreditation standards is a key benchmark for hospitals and psychiatric facilities to ensure that deficiencies are identified and services provided to patients are consistent with professional standards, with an aim of continuous improvement.
To dismiss prisoners’ legitimate criticisms about limited access and quality of mental health care, the CSC has repeatedly used accreditation as a shield to respond to such concerns. Accreditation is important but should never be used as a shield – accreditation does not, for example, set standards on the appropriate patient/mental health professional’s practice and minimal level of mental health care. CSC Communications should never use accreditation to dismiss legitimate concerns.
RTC Population Profile
In a 2024 profile of mental health care patients 6, CSC provided the following demographic information for the 498 individual patients in custody at all RTCs (see Table 2). According to their data, the vast majority of RTC patients are men (98%), more than one third identify as Indigenous (34%), and the majority are classified as medium or maximum security (62% and 24%, respectively). As for diagnoses, 86% of individuals at an RTC had at least one mental health diagnosis, with the most common being schizophrenia (46%), followed by depression (15%), anxiety disorder, and opioid use disorders (12% respectively).
Table 2. Demographic and Diagnostic Profile of RTC Patients (n = 498)
| # | % | |
|---|---|---|
| Gender | ||
| Male | 487 | 98 |
| Female | 11 | 2 |
| Race | ||
| White | 248 | 50 |
| Indigenous | 167 | 34 |
| Black | 32 | 6 |
| Other | 51 | 10 |
| Security Level | ||
| Maximum | 118 | 24 |
| Medium | 310 | 62 |
| Minimum | 45 | 9 |
| No rating | 25 | 5 |
| Mental Health Diagnoses | ||
| Schizophrenia | 227 | 46 |
| Depression | 77 | 15 |
| Anxiety disorder | 59 | 12 |
| Opioid Use Disorder | 58 | 12 |
| Borderline Personality Disorder | 40 | 8 |
| Post Traumatic Stress Disorder | 40 | 8 |
| Dementia | 26 | 5 |
| Fetal Alcohol Spectrum Disorder | 21 | 4 |
Note. The numbers for diagnoses exceed the total as individuals may have more than one diagnosis.
Previous Reporting on RTCs
While the Office had not examined RTCs at an in-depth level prior to the issues that emerged from the Bissonnette investigation, we had previously raised several concerns regarding their overall purpose and admission criteria more than a decade ago.7 In more recent years, the Office has flagged issues regarding excessive use of force at RTCs, recommending a review of security practices and protocols to ensure a more supportive clinical environment. Most notably, the Office’s 2017-2018 Annual Report provided a summary of the findings from an independent expert review conducted by Forensic Psychiatrist, Dr. John Bradford.8 Some of Dr. Bradford’s findings included concerns regarding a lack of adequate training for staff working with forensic patients, a complete disregard for the selection of appropriate correctional staff to work in this type of environment, problematic infrastructure, poor assessment tools and admission criteria, and the growing problem of meeting the needs of aging patients. Overall, Dr. Bradford concluded that the infrastructure, staffing, and operational models in place at RTCs at the time did not adequately meet the complex needs RTC patients.
Given these findings, the significant problems raised in last year’s Annual Report, and the thematic focus on mental health for this year, a comprehensive examination of these RTCs on a broader, more systemic level was necessary.
Current Investigation
For the current investigation, I instructed my staff to conduct an in-depth review of CSC’s Regional Treatment Centres. Multiple areas of focus were explored, including but not limited to the governance structure, staff selection and training, the dynamic between security and health care, the quality of mental health care, infrastructure, challenges of the ‘hybrid’ model, deaths in custody and related NBOIs, and examples of promising practices. We employed a range of investigative methods and relied on multiple sources including:
- on-site inspections of each of the five RTCs, including my own visits;
- visits to other forensic hospitals and provincial treatment facilities;9
-
interviews with 150 current and former CSC staff, external stakeholders, and patients;
- CSC staff interviews consisted primarily of RTC senior and middle managers, mental health and health services professionals, and frontline health and operational staff. For co-located penitentiaries, senior managers were also interviewed; and,
- reviews of literature, data, and CSC policy instruments relating to RTCs and mental health.
A total of 12 OCI staff supported the efforts of the current investigation, which was further strengthened by participation from an external subject matter expert and former CSC psychologist and National Investigator. Further to these efforts, the following findings were identified:
- Outdated and inappropriate infrastructure for a psychiatric and therapeutic hospital setting.
- RTCs have become holding centres for the growing number of aging and infirm persons behind bars.
- Security responses take precedence over the delivery of physical and mental health care.
- Over-reliance on the use of force on patients, including the concerning use of OC (oleoresin capsicum) spray as a means to interrupt self-injury.
- Weak governance structure and absence of national policy lead to role confusion and the undermining of clinical decision-making by mental health professionals.
- A lack of specialization required in the recruitment, selection, and training of staff.
- The “stabilization” of behavioural symptoms of mental health appears to be the overriding objective of co-located RTCs.
- Per a review of NBOIs, CSC has systematically failed to learn from or prevent numerous serious incidents and deaths.
- The marked absence of dedicated patient advocates in RTCs infringes on patients’ rights and needs.
Our findings revealed that the long-standing issues and concerns previously raised by this Office and Dr. Bradford are still present today. Additionally, in the context of an aging and increasingly complex population, conditions have arguably worsened since the last reporting on RTCs occurred. These facilities are not positioned to provide specialized, psychiatric hospital care, particularly to those with severe levels of mental and physical needs. At best, they are offering what would be expected of intermediate levels of care for the purposes of stabilization, not longer-term treatment or care. Despite being referred to as Regional Treatment Centres, these facilities essentially amount to penitentiaries offering psychiatric services with limited capacity for emergency care. None of the RTCs live up to their name, nor can they be considered to be classified as a proper psychiatric hospital.
Findings
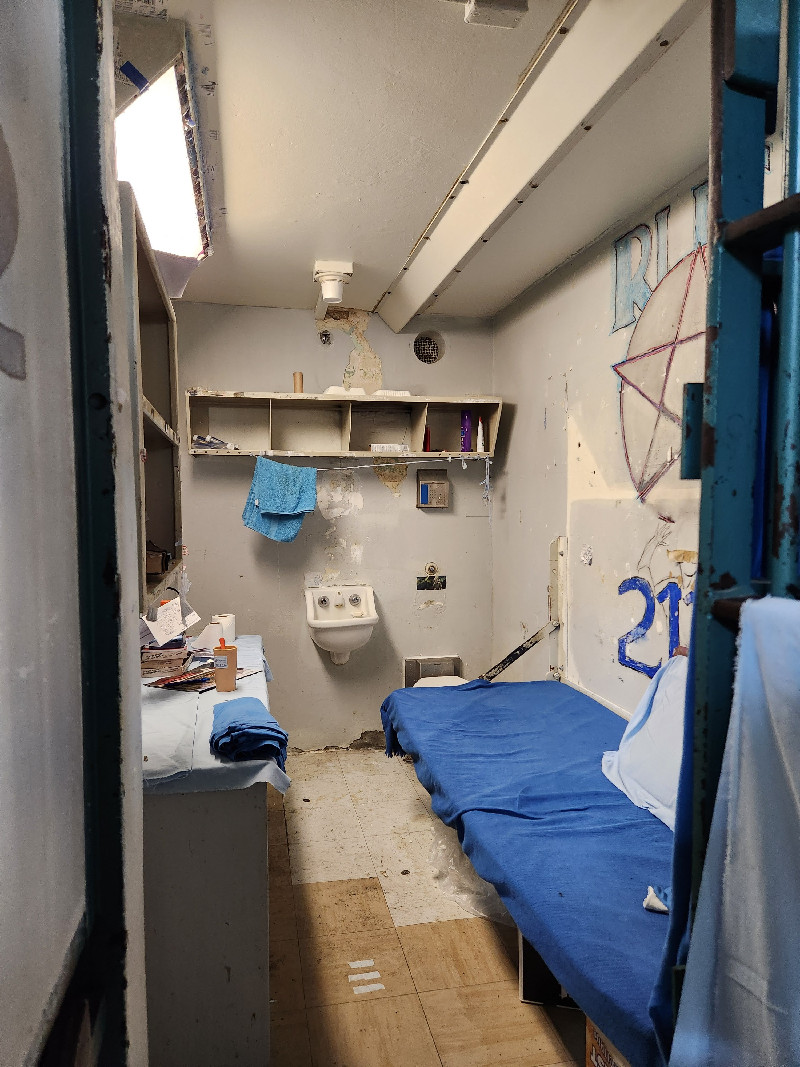
1. Outdated and Inappropriate Infrastructure for a Psychiatric Hospital and Therapeutic Hospital Setting
The majority of the individuals interviewed for this investigation were asked a fundamental question: Is this facility a prison or a hospital? From an environmental standpoint, that answer is all too obvious. By and large, these centres look and feel no different from any other federal institution. As one Warden put it, “When you walk around the institution, I’ll let you be the judge.”
Furthermore, the age and design of the infrastructure was raised by a large proportion of staff when asked about the biggest challenges they face in providing services in a correctional treatment centre. The Shepody Healing Centre, for example, is found within the walls of Dorchester Institution, constructed in 1880 as a maximum-security institution and currently the second-oldest Canadian penitentiary in operation. Consequently, psychiatric patients are confined to units lined with cramped, barred cells, offering limited treatment and program space. Health care staff charting and discussing patients’ cases must do so in congested control modules, mere feet away from correctional officers. Privacy concerns aside, this proximity is symbolic of an ever-present influence of security staff on the health and mental health disciplines at each of the treatment centres.
The RMHC for instance, forms part of Archambault Institution, originally constructed as a maximum-security institution. RTC (Ontario), comprises two separate 96-bed units, one on the grounds of Bath Institution (medium security) and the other housed at Millhaven Institution (maximum security). As the Office has previously reported, the design of these units can be found in numerous institutions as it lends itself to the convenience of rapid tendering and construction. Elsewhere, this “copy-paste” model has been repurposed to include Structured Intervention Units, Therapeutic Ranges, integrated/non-integrated maximum-security ranges, and transition ranges. As in each of these other applications, RTCs using this design lack sufficient space to provide clinical interventions, programs, education, and Indigenous services. As one Warden described it, “When you plop patients in a 96-man unit and call it a treatment centre, that’s not right. It is not conducive to a therapeutic environment at all.”
Even the only standalone, purpose-built RTC, the Regional Psychiatric Centre, in Saskatoon, which occupies leased property from the University of Saskatchewan, is not immune to the traditional fixtures of a high-security institution. Barbed wire now lines the inner courtyard of the institution, in response to an attempted escape in 2019, despite resistance from the University due to the negative impact this would have on the reprieve the courtyard previously afforded patients. A psychiatrist we interviewed provided significative reflections: “This place was supposed to be a unique facility. It was established to provide high-quality care and be a leader in forensic mental health, clinical teaching, and rehabilitation. It was not designed to be one of the RTCs. We’re not supposed to run just like a penitentiary. This is a prison, with the opportunity for treatment.”
Some modifications have been made to existing infrastructure as attempts to accommodate certain segments of the patient population, such as elderly individuals and those with mobility issues. At the RTC Pacific, for example, the geriatric unit has been retrofitted with larger doors and hospital beds. Despite these changes, all five facilities are structurally and environmentally unsuitable for proper therapeutic or accessibility- minded care.
The Health Centre of Excellence
In the course of this investigation, inquiries were made to identify whether any plans were underway to address these long-standing and well-known infrastructure problems. In response to an information request, CSC relayed that its Technical Services and Facilities Branch is currently in the process of developing new standards for RTCs and therefore halting any new construction, major capital projects, or redevelopment of master plans for all but one facility. The exception is the Shepody Healing Centre, which has long been slated to be replaced by a planned new Health Centre of Excellence (HCoE).
Our Office attempted to obtain more information about the planned HCoE, which was first announced in 2018 as a “national resource” to meet the increasingly complex needs of the patient population.10 Since then, expected costs for the project have ballooned from $300-400 million to approximately $1.3 billion, representing the largest federal investment in New Brunswick since the construction of the Confederation Bridge in the mid-1990s. While CSC has been reluctant to divulge plans for this facility to our Office, information has periodically been shared with the general public over the several years since the project was first announced. For example, on December 19, 2024, the Minister of Public Safety at the time, Dominic Leblanc, confirmed during a press conference that the HCoE will include 150 beds, nearly triple the existing capacity of the Shepody Healing Centre. It will offer bilingual services and accommodate both men and women, including aging patients and those with physical disabilities. Apart from these details, little has been revealed regarding the guiding philosophy, approach to the provision of care, recruitment of suitable staff, etc. that would make this a “Centre of Excellence” that distinguishes itself from the existing RTCs and model.
The project, which has seen multiple delays since its announcement, at the time of this writing, is at the Request for Proposal stage to identify a suitable contractor. While there is a consensus that the Shepody Healing Centre is in dire need of a replacement, the cost of the HCoE is staggering and, as this Office has recommended in the past, CSC should not be in the business of building new, expensive, state-of-the-art options to house individuals requiring significant mental and physical health care. Corrections and specialized mental health care should never be under the same umbrella. This approach is inconsistent with the United Nations Standard Minimum Rules for the Treatment of Prisoners (Nelson Mandela Rules). 11
This Office has seen no evidence to suggest that the HCoE will fundamentally operate any differently than the current RTC model, despite our requests to see such plans. Seven years after its announcement, an empty field next to the existing penitentiary sits idle, awaiting an eventual groundbreaking. The concerning reality is that until the HCoE is operating, patients will continue to be housed in a facility that is grossly inappropriate and inconsistent with a treatment centre, which CSC itself has acknowledged. According to documents provided by CSC, the design and construction phase is expected to extend to 2032. Other than the HCoE, any new construction or major capital projects related to RTCs will be deferred until the new standards are in place, at which point, master plans for the remaining facilities containing RTCs or equivalents will be revisited.
2. RTCs have Become Holding Centres for the Growing Number of Aging and Infirm Persons Behind Bars
“The aging population is another issue. I get lots of referrals for individuals who don’t belong in a hospital bed, are simply aging, and require intravenous medication.”
Chief of Health Care
According to CSC, while 82% of those serving time at a treatment centre have had a mental health diagnosis, 30% of individuals at RTCs do not actually meet CSC’s own criteria for admission (i.e., do not have a Mental Health Needs Scale on file indicating considerable or high needs). These individuals have been admitted to an RTC largely on the basis of “exceptional admission” – individuals with serious physical disabilities who require 24-hour nursing or other clinical care not available in the region. Most common among these are age-related ailments, including hypertension, hepatitis C, tuberculosis, diabetes, dyslipidemia, osteoarthritis, Chronic Kidney Disease, and Chronic Obstructive Pulmonary Disease.
As it stands, the RTCs house a significantly older and infirm population compared to other federal institutions. Specifically, the proportion of individuals over 50 years of age accounts for 42% of the RTC population overall, compared to 26% of their co-located facilities. Individuals aged 65+ represent 25% of individuals in RTC beds, while only accounting for 7% of those in the mainstream facilities. This Office has previously reported on the growing number of aging individuals in federal custody, putting forward recommendations to both the Service and Government to increase release options for the aging and dying, to enhance partnerships with specialized community service providers, and to significantly reallocate existing institutional resources to community corrections to better support the reintegration needs of aging offenders. When walking through these units, it is blatantly evident that these patients would not pose any undue risk to society and could be easily and safely managed in the community, in keeping with CSC’s legal obligation to apply the “least restrictive measures” when administering sentences.
The number of individuals over the age of 50 in federal corrections has continued to increase year-over-year and will continue to do so. Given this trend, the infrastructure and services in place are grossly inadequate to humanely meet the needs of this population. For example, RPC’s psychogeriatric Mackenzie Unit has physical infrastructure challenges, including cells built in the 1970s, without anticipating the room required or unique needs of a geriatric population. Older patients suffering from conditions such as incontinence and needing a brief change, for example, find themselves restricted by institutional routines, including security patrols, designated cell time, or formal counts. These conditions are detrimental to patients’ health and wellbeing as well as to their right to dignified care.


With the growing needs for both physical and mental health care, and the co-occurring nature of these issues that come with age, CSC needs to contend with and resolve the growing demand for specialized care. Quality of care aside, at present, choices are being made and exceptions are being granted for those with pressing physical care needs, which in turn means that many who require psychiatric care remain in a mainstream facility due to a lack of bed space at the RTCs. According to CSC, 3% of the in-custody population meets the criteria for admission to an RTC but are not in an RTC bed. These individuals are mostly in maximum security, are Indigenous individuals, and/or are women. It is our understanding the CSC Health Services sector is currently undergoing an initiative to not only standardize services across RTCs, but to also develop a plan to address these ever-mounting pressures. This Office awaits the outcomes of this much-needed exercise.
3. Security Responses Take Precedence Over the Delivery of Physical and Mental Health Care
“To understand the philosophy of care that has evolved in the treatment centre, one only needs to look at the complement of staff. At the inception of the treatment centre, the staff complement of COs [correctional officers] to nurses was approximately 50 COs to 100 nurses, and nurses were responsible for both physical care and mental health intervention programs, they knew their patients well. At present, there are approximately 130 COs to 48 nurses. Because of the direction that CSC has chosen to take, the treatment centre feels more like a prison today than it ever did.”
Psychiatrist
Unjustifiable Emphasis on Security Measures and Perceptions of Risk
Despite the inclination to impose high security measures and often treat these facilities as maximum-security due to their collocation or presence of maximum-security patients, in reality, they see less gang involvement and violence. Security Intelligence Officers play a different role, as issues such as the introduction of contraband and the presence of Security Threat Groups (STGs) are far less pronounced. One Warden explained that gang membership becomes less of a determining factor at RTCs once individuals realize that they do not have to adopt the same identity as they might in a mainstream institution. He remarked further that “STG guys realize that they don’t need to live up to the label that we, the organization, gave them.”
Over the past five fiscal years, RTCs saw 961 incidents of possession of contraband,12 which represents less than 2% of all incidents of possession of contraband during that time. In fact, staff reported that the diversion of medication, including Opiate Agonist Therapy such as Suboxone, poses far more of a problem in these facilities than traditional contraband found in other mainstream institutions. The diversion of medication by patients involves misdirecting or misusing prescribed medication for personal use or reselling. For example, a Warden noted that “We don’t have an issue with drones here. I’m a big pharmacy. Patients can get whatever they want by talking to a doctor.”
Nevertheless, there is no question that working with a complex, occasionally volatile population carries an inherent risk. Over the last five fiscal years, RTCs saw 34 attempted suicides and nearly 1,500 incidences of self-inflicted injury. During the same period, three patients died by suicide.13
Physical Barriers to Staff-Patient Interaction and Dynamic Security
Violent incidents, including assaults on staff, do occur and can often precipitate the imposition of additional security measures, impacting both physical structure and routine. There is a predominant narrative that correctional staff are “responders,” which, in principle, is counter to the notion of early identification, intervention, and dynamic security, all of which are crucial in a mental health facility. It is unsurprising then, that health care staff at sites where this sentiment is most discernible tend to mirror their correctional counterparts. As an Executive Director frustratingly remarked, “A lot of our nurses wear epaulettes now.”
While the instinct to fortify a correctional facility can be understood, some disproportionate safety measures, often in the form of physical barriers, come at great expense to staff-patient interaction, observation, therapeutic rapport, and dynamic service delivery. When face-to-face interactions between patients and staff, whether scheduled or spontaneous, are limited by structures, access to and quality of care are significantly curtailed.
Nowhere was this general attitude and regression more obvious than at the RPC in Saskatoon, where both correctional and health care personnel have increasingly withdrawn from the units, completing more of their duties in control modules and enclosed nursing stations. At the centre of RPC’s Bow Unit, for example, a horseshoe- shaped workstation, originally designed to promote direct observation and interaction with patients, sits abandoned in favour of an inner module and a newly constructed floor-to-ceiling glass partition that puts distance between staff and patients. During our inspection of this unit, negotiation was ongoing with the union representing nursing staff after they were encouraged by management to leave their enclosed nursing station for 15 minutes a day to be more visible to patients, resulting in resistance and demands for more physical barriers.
Compounding security issues, the RTCs are considered to have a multi-level security designation. Commissioner’s Directive 706 - Classification of institutions defines some of these parameters and behavioural expectations as follows:
Security
- The perimeter of the Regional Treatment Centre will be well defined, secure and controlled. Firearms will be retained in the treatment centre and will be utilized for perimeter security. However, they will only be deployed inside the treatment centre during emergency situations with the authorization of the Institutional Head.
Behavioural Norms
- The behavioural norms for inmates at Regional Treatment Centres will reflect their security level, and inmates are expected to comply with their treatment plan and Correctional Plan.
In practice, this means that patients with an Offender Security Level consistent with minimum, medium, or maximum security can be admitted to an RTC from institutions with any of the aforementioned security levels. Once admitted to the RTC, patients may find themselves on living units with individuals previously found to have presented a higher security risk. While managing the complexity of such a population can be a point of pride for some, this typically contributes to the security-focused culture that permeates the RTCs, as correctional staff appeared to focus on the presence of, traditionally classified, maximum-security individuals and therefore default to treating the institution as if it were maximum security. Coupled with the structural trappings of a prison environment, this general attitude makes these facilities feel even further removed from what one would expect from a psychiatric hospital. A psychiatrist characterized the dynamic found at RTCs by stating that “Operational concerns always outweigh clinical concerns.”
While less commonplace than in mainstream institutions, decisions to impose lockdowns are also purely operational, and include little to no clinical consultation on the potential impacts that they can have on the patient population and quality of care. At one site for example, psychiatrists shared that patients were locked in their cells for most of the workday, leaving approximately two hours in the morning and two hours in the afternoon for patients to be seen by psychiatry, mental health staff, nurses, parole officers, and/or to participate in programming. Furthermore, the presence of security staff on a unit was viewed as so essential to the operational routine, and that if not appropriately staffed with correctional officers, an entire unit would be locked down. That is, patients were locked in their cells, regardless of how many health services staff were on the unit, prepared to see patients.
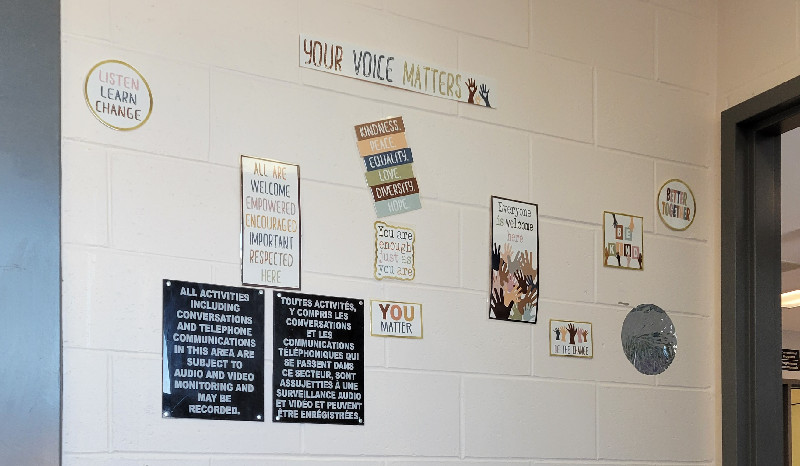
Cultural and Attitudinal Barriers to Staff-Patient Interaction and Dynamic Security
“The problem is how the language has changed. Even nurses now say inmate instead of patient. If you don’t fit the culture, it spits you out.”
Psychiatrist
"We are sometimes told by the officers, ‘Hey you’re in a pen here’ [...]. Before, if you said ‘I want to see Mr. So-and-so’, you were told that he was not a ‘Mr.’ [...] of course, here you have to find your place without confronting them and I know very well that I can’t give orders to officers."
Nurse
The pervasive reminders that one is in a prison are not only visual, but also extend to the language used by institutional staff in reference to those residing there for treatment. Throughout the course of the investigation, these individuals were continually referred to as “inmates” rather than “patients” by all correctional staff we interviewed. While less frequent, mental health professionals, including psychologists and psychiatrists, occasionally made this distinction, before correcting themselves.
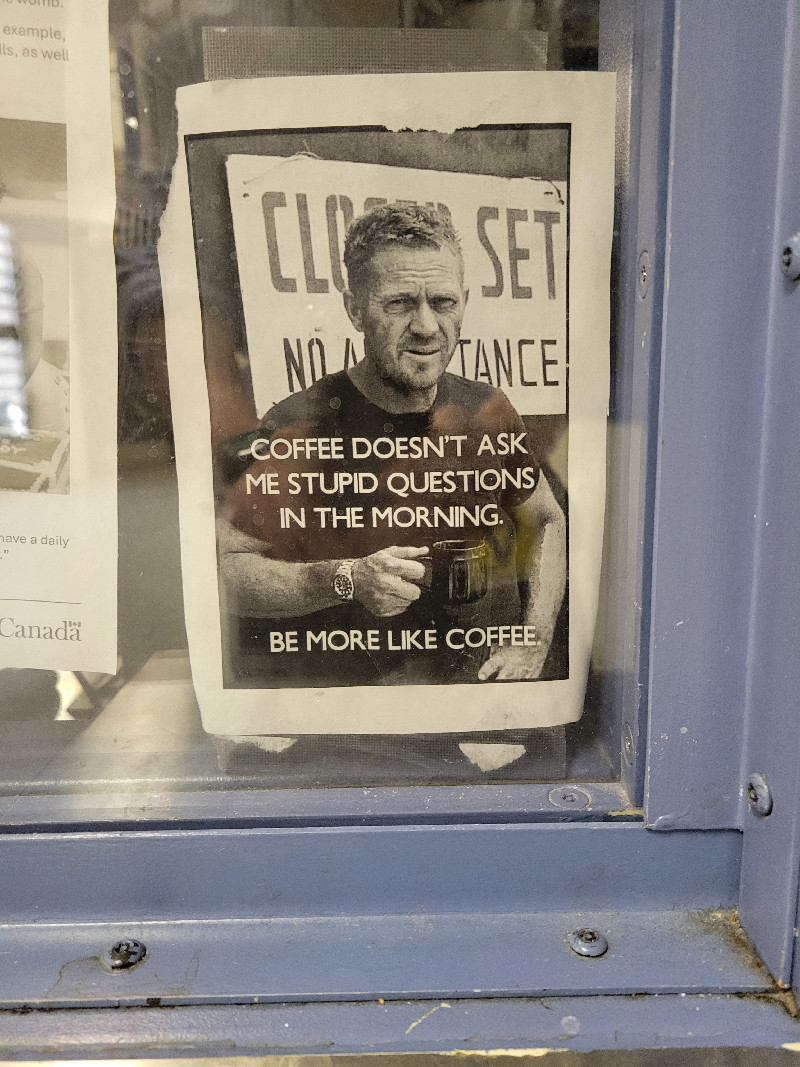
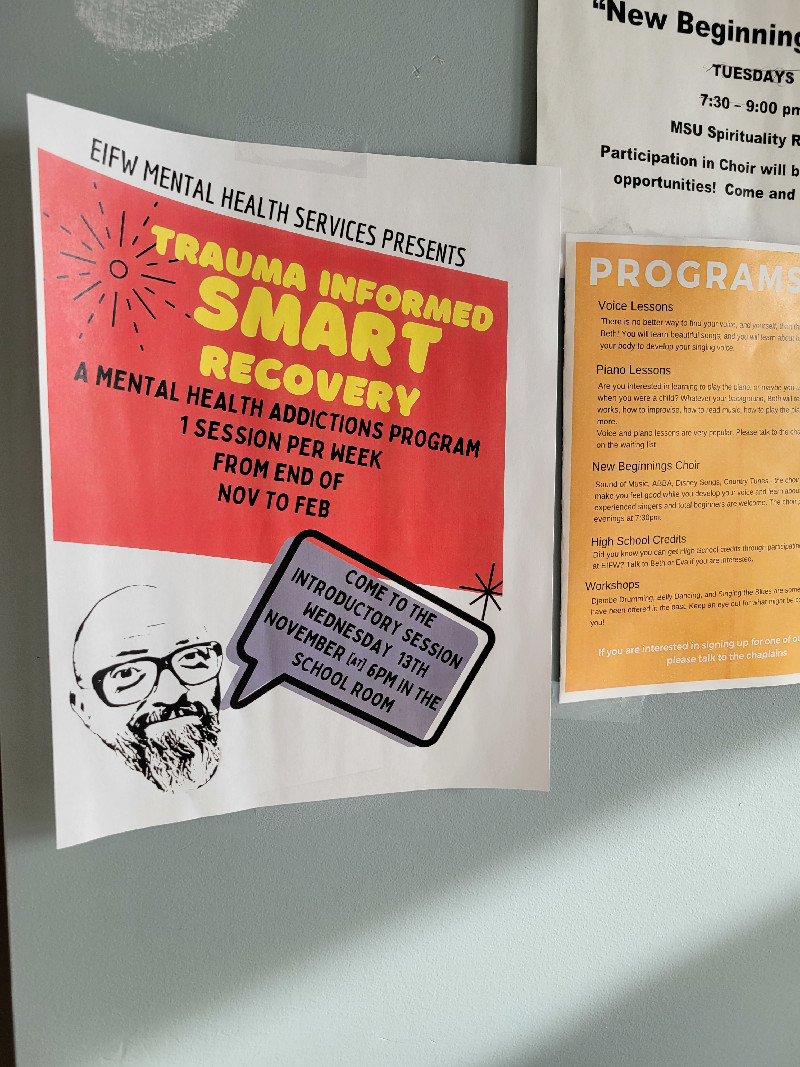
The influence of culture, attitudes, language choice, and perceptions of “inmates” versus “patients” can impose considerable barriers to treatment. This dynamic was evident at all RTCs. The encapsulation of such attitudes was evidenced by a strategically placed poster found near a medication window within the RPC’s Bow Unit control module. The poster was taped on the inside of the structure’s plexiglass with the picture and print facing the patients, the message to patients read as follows:
The othering, belittling, and/or dehumanizing of patients with complex mental health needs in an “accredited psychiatric hospital” is simply unacceptable. This stands in stark comparison to the manner in which security concerns are managed and addressed, and patients are viewed, in provincial forensic psychiatric treatment centres and hospitals whose patient profiles also consists of those with complex mental health needs who, at times, exhibit volatile behaviours. The provincial forensic psychiatric centres we visited informed us that the first point of contact for all patients are health services and mental health professionals. In fact, their security partners are not present on units, do not manage movement, and do not conduct rounds, all of which are commonplace in a federal treatment centre. Rather, at the first indication that a patient appears to be struggling or showing signs of distress, health services and mental health staff engage the patient, in an effort to avert, manage, and/or stabilize the individual.
The ability to foresee and observe signs of distress or decompensation requires significant familiarity, observation, and interaction with patients - a full-time, round-the-clock job. Only as a very last resort, when a patient is aggressive, should security partners be called for assistance. Their role at the time of their arrival is clearly conciliatory and de-escalation with physical handling should be used only if required to ensure patient and staff safety. Of course, the ability to foresee and observe signs of distress/decompensation and to avert aggressive behaviour is not always possible. Provincial forensic psychiatric hospitals have had their share of incidents when health services staff were harmed, or a patient has escaped. Despite this, they have remained loyal to their mission and mandate of being a psychiatric hospital and held back from quickly using static, security-focused solutions. These facilities stand as proof-of-concept that correctional treatment centres can be run in a health-first manner, when there is the organizational will, commitment, and support of such a fundamental philosophy and operational approach.
For example, following an escape at one of these provincial forensic facilities, and despite pressure to install razor wire, the potential for a patient to be ensnared, entangled, and mangled in razor wire factored heavily in their deliberation of options. Alternatives were therefore explored and resulted in a “candy-cane” fence being installed – a fence that has an aluminum casing at its top, in the shape of a candy cane – that makes future escapes difficult, but results in less risk to patient safety. Similarly, following incidents of staff being physically harmed, the hospitals increased training and developed more effective de-escalation skills, initiated meaningful (internal and external) reviews of the incidents which they used as an organizational learning tool. Recommendations from such reviews, particularly those that benefited the welfare and safety of the patients and the public, were welcomed – rather than dismissed.
While some RTC staff noted that a perceptible decline in dynamic security has been steady and long-standing, some staff were of the opinion that the onset of the COVID-19 pandemic also saw a significant shift in this dynamic. Staff suddenly perceived patients as an additional risk to them and their families. As a result, the quality and quantity of interactions diminished. This reversal in dynamic security and patient engagement mirrors the trend that the Office found in its investigation of men’s standalone maximum-security institutions in 2023-24 14
A Clash Between Operational and Health Care Sectors
“Governance is a huge issue. The current model is awful. Health policy is very clear; Operations policy is very clear; but Regional Treatment Centre policy is non-existent. It does not allow us to work in the grey.”
Warden
“I strongly believe that we need our own policy. We try to be health and operations and the two do not work together. We’re driving down different roads but are we going to the same place?”
Deputy Warden
“There’s always a bit of disagreement here. There is a gap between health and operations and the balance between the two remains fragile. This has an impact on the working climate.”
Correctional Manager
Increases in the securitization of treatment centres (infrastructure, protocols, and staff culture), coupled with decreases in dynamic approaches to security and treatment, are further hampered by clashes between health care and operational sectors. In the course of this investigation, perhaps one of the best illustrations of this rift emerged following the release of a case report from the Office of the Public Sector Integrity Commissioner (PSIC) in March 2020, which found that “CSC neglected to take adequate action to stop acts of insubordination, and harassment and intimidation by several Correctional Officers against other employees within the Regional Mental Health Centre (RMHC), at the Archambault Institution.”15 The report detailed systemic harassment by RMHC correctional officers directed toward mental health professionals working on the units and various managers, due to the desire of the correctional officers dictating where a psychologist was allowed to see a patient.
In protest of management’s support for the psychologist to provide counsel to the patient in their office, a correctional officer assigned to the RMHC left his post. This left several RMHC employees locked in offices with patients with no nearby support for nearly 30 minutes, while a nurse was locked on a range full of patients in a similar predicament. The PSIC report documented the following examples of harassment:
“Some Correctional Officers displayed a children’s teddy bear as a pejorative reference to the work of RMHC employees.
Some Correctional Officers made and displayed banners with discriminatory messages that belittled and mocked the RMHC inmates with mental health issues and the work of RMHC employees.”16
The events, coupled with related and unrelated acts of insubordination, racism, and intimidation by the correctional staff toward colleagues, are a clear example of the fundamental difference in perspective about security versus patient care. During the current investigation, similar accounts emerged. For example, two mental health professionals we interviewed at one treatment centre recounted that approximately two years prior, correctional staff tried to convince patients on a unit that a dog was present, going so far as to bring in a bowl of water and dog food for the sole purpose of confusing patients for their own amusement.
With respect to the sharing of personal health information between these groups, it is evident that there is a differing and oftentimes poor understanding of what can or needs to be shared both on an interdisciplinary level and with operational staff. Given the interdependence of health care, mental health, and operations, it is essential to share crucial information about patients to ensure their safety and effective treatment. One would therefore expect to find more clarity when it comes to the “need to know” principle. Yet, at each of the RTCs, staff expressed confusion and frustration about what was being shared.
4. Over-Reliance on the Use of Force on Patients, Including the Concerning Use of OC Spray as a Means to Interrupt Self-Injury.
This Office has repeatedly raised concerns with the use of force in federal institutions since the Engagement and Intervention Model (EIM)’s implementation in January 2018, particularly as it relates to the Service’s supposed focus on prioritizing non-physical and de-escalation responses to incidents and the incorporation of health care into the new EIM. Moreover, the use of force on vulnerable individuals, including those suffering from mental and physical issues has caused further alarm and runs counter to the recommendations put forth by CSC’s own 2021 evaluation of the EIM.17 For context, from April 2024 to January 2025, there were a total of 195 unique use of force incidents involving 137 incarcerated individuals at the five RTCs and nearly 1,000 such incidents through the last five years.18
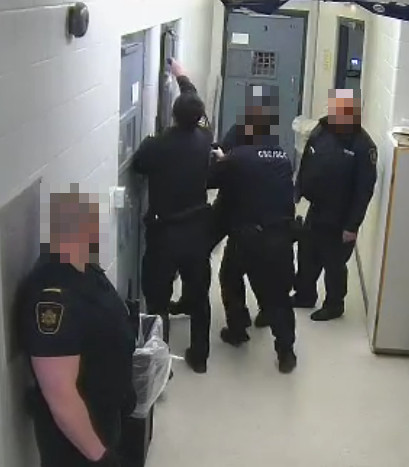
Despite an identified need to employ alternatives to force with this segment of the population, patients are more likely to encounter force than in a mainstream institution. While only accounting for approximately 4% of the total federal custodial population, use of force incidents at RTCs accounted for 10% of all use of force incidents in federal corrections in 2024-25 (195/1,908), and 11% of all use of force incidents in the last five years (994/8,777). The rate of use of force incidents at RTCs in 2024-2025 was 38 per 100 individuals, compared to an overall rate of 12 incidents per 100 individuals at all other institutions. Despite some minor fluctuations, this rate has remained relatively stable over recent years.
Perhaps related to their distinct profiles or collocation, use of force incidents do not occur uniformly across the RTCs. For example, in 2024-25, most use of force incidents occurred at RTC Millhaven (41.5%), followed by RPC Prairies (34%). With respect to the types of incidents that result in force being used, in 2024-25, the primary causes were the following:
- 37% of the use of force incidents were in response to an assault-related event
- 35% were in response to “behaviour-related issues”
- 21% occurred in response to incidents of self-harm
Over the same period, the primary types of force used at RTCs were restraints (54%), non-inflammatory/non-lethal force (26%), and inflammatory sprays/munitions (18%), the latter of which is of particular concern to our Office in the context of incidents involving self-harm. If we consider the last five fiscal years, of the total (366) use of force incidents that occurred at RTCs in response to self-injurious behaviour or attempted suicides, inflammatory sprays/munitions were used in 38% of cases (139/366). Examples outlining various responses to use of force situations in RTCs can be found in the Appendix that follows the conclusion of this report.
While troubling, it should be noted that there was a total of 1,534 incidents of self-injury and attempted suicide at RTCs during this period of time. This means that, force was used in approximately one quarter (24%) of these incidents, and therefore, inflammatory spray/munitions were used in 9% of all recorded incidents of self-injury or attempted suicide overall. While incident-level analysis would be warranted to determine the appropriateness of measures and types of force used, it is nevertheless our view is that this level of force should only be reserved for the most exceptional circumstances of acute mental distress or crisis, as a last resort. Although individuals at treatment centres may present with more complex issues, one would expect fewer uses of force and greater reliance on therapeutic responses or de-escalation techniques, as illustrated in the community/provincial correctional forensic hospital examples that follow.
The major difference between a CSC-operated RTC and provincial or community forensic hospital is who is considered to be the first responder. By and large, correctional officers play this role in CSC facilities, particularly during evenings and weekends, whereas provincial and community forensic counterparts tend to rely on mental health professionals to act at as their default frontline staff in these situations.
Effective Alternative Approaches to Security in a Psychiatric Correctional Setting
St-Lawrence Valley Correctional and Treatment Centre
At the St-Lawrence Valley Correctional Treatment Centre, a Schedule 1 psychiatric facility co-operated by the Ontario Ministry of the Solicitor General and the Royal Ottawa Mental Health Group, the frequency of incidents among residents admitted to the Secure Treatment Unit is mitigated by the use of formal behavioural contracts. Residents enter these contracts with the understanding that failure to meet expectations can result in their discharge and, conversely, adherence to the contracts can earn them various privileges. When conflicts between residents or staff occur, significant efforts are made to engage in mediation and dispute resolution, often in the presence of clinicians.
By design, correctional staff are not visible on the units and the vast majority of day-to-day operations are managed by health care and mental health professionals. They seldom conduct security patrols on the units, focusing instead on perimeter security, and primarily act in response to serious incidents. Our staff learned that the concerted effort to remove the static- security influence and response of armed, uniformed officers in a treatment milieu was successful and enhanced the therapeutic aspect of the treatment centre. In the rare event that a resident needed to be placed on a fixed-point restraint bed, negotiation was done exclusively by nursing staff and similar health care personnel. Moreover, when residents were placed under constant supervision because of a risk of suicide or self-harm
Institut national de psychiatrie légale Philippe-Pinel (INPLPP)
Much like St-Lawrence Valley, the INPLPP, employs a conscious approach to integrate both dynamic and static security measures. Again, static security measures and the presence of security are kept out of patient sight as much as possible. Dynamic security (i.e., persistent/sustained interaction with patients) is at top of mind, as the INPLPP emphasizes and prioritizes the need for staff to get to know patients in order to identify crises early, offer supports, and intervene while remaining cognisant of security concerns.
5. Weak Governance Structure and Absence of National Policy Lead to Role Confusion and the Undermining of Clinical Decision-Making by Mental Health Professionals.
Muddled Decision-Making
In the Office’s 2023-24 report on the death of Stéphane Bissonnette at RTC Millhaven, we outlined the conditions that Mr. Bissonnette frequently found himself in. These included numerous placements in the Pinel Restraint System (PRS) and his placement on a Modified Suicide Watch at the time of his death. These are some of the most restrictive conditions a suicidal or self-injurious patient can be subjected to, intended to be used as a last resort if all other measures to cease the behaviour have been unsuccessful. The PRS consists of variable point restraints (up to seven), typically affixed to a bed, used to immobilize portions of patients’ bodies and limbs fully or partially. Enhanced observation measures, such as Modified or High Watch, involves making the decision to place an individual in a specially designed observation cell, under continuous observation by staff, either directly or via CCTV. Patients are often stripped and made to don specially made anti-suicide security gowns.
This investigation found that policy outlining where decision-making authority lies in the event of self-injurious or suicidal behaviour, Commissioner’s Directive 843 - Interventions to Preserve Life and Prevent Serious Bodily Harm, leaves much to interpretation at the site level. Confusingly, despite the presence of trained mental health professionals and an Executive Director at each RTC, the decision to place or remove patients in the Pinel Restraint System rests with the Institutional Head, unless the Executive Director has been identified as a designate. The same applies to the initial placement of patients on High Watch or Modified Watch and subsequent modifications to the conditions. We found that in only two Standing Orders was the Executive Director explicitly identified as the designated authority to make such decisions. Multiple psychiatrists reported that despite being on call after hours, such decisions, which they deem to be psychiatric in nature, can be made by operational staff such as Correctional Managers in charge of institutions after daytime hours, only for them to be apprised after the fact. While this can be in keeping with the overarching directive, there is disagreement over the experience required to make such decisions.
Standing Orders stemming from CD 843 vary significantly across institutions19. Notably, discrepancies exist in decision-making responsibilities for High Watch and Modified Watch. For instance, the Executive Director is responsible for decisions at some RTCs, while at others, it is the Warden who oversees the placements or any subsequent modifications. Furthermore, the lack of clarity and inconsistency in directives regarding responsibilities outside of regular hours are noticeable and could lead to delays in interventions and general misinterpretation. The use of the Pinel Restraint System also shows variation in authorization and decision-making procedures, especially regarding mental health personnel’s involvement: while some institutions require consultation prior to intervening, others do not provide any specificity on that matter, or the instructions within the Standing Order allow for a high level of discretion. Moreover, Mental Health Monitoring, another observation status, is generally overseen by health care professionals, but specifics may vary, again, especially regarding responsibility outside of regular hours.
In practice, we found that decisions to place individuals in these restrictive conditions were undertaken differently, depending on the treatment centre and willingness of either the Warden or Executive Director to assume this role. For example, a Warden we interviewed described his apprehension upon assuming the role and being faced with being the decision-maker for such clinical matters, noting that there was no support to help inform his authorization and that he had to resort to seeking out mental health professionals for guidance. Another Warden plainly explained that his background, largely in correctional operations and interventions, did not provide the experience needed for this sort of assessment and decision. Taking these sorts of decisions out of the hands of trained mental health professionals serves to undermine their experience, judgement, and clinical expertise, leading to resentment, burnout and infighting among staff. Medical staff at the RMHC, for example, some of whom work in outside hospitals and forensic environments such as the Pinel Centre, reported that they have less professional autonomy in the treatment centre due to the governance structure and policies currently in place.
Absence of Specific RTC Policy
“The [Commissioner’s Directives] have nothing to do with quality of patient care. As a starting point, the CDs are fine, but they have to go beyond that. People, especially new staff, will stop at compliance with the CDs.”
Chief of Health Care
One of the clearest indications of the muddled governance structure in place is the absence of policy instruments specific to the RTCs. A policy specific to the treatment centres can subsequently drive helpful and site-specific Standing Orders, while maintaining an emphasis on patient care and mental health.
Because of the unique nature of co-located facilities, those RTCs and their shared facilities also share a roster of correctional staff. In practice, this can mean that a correctional officer who typically works in a prison, such as maximum security Millhaven Institution, can be deployed to work in the adjacent treatment centre. While some correctional staff express a genuine interest and willingness to work in the area of mental health, this depends on staffing needs and seniority, as per the Global Agreement between CSC and the Union of Canadian Correctional Officers.20 Recruitment and deployment issues are not unique to security staff, as nursing staff at collocated sites are often reluctant to accept posts in the RTC or vice versa, causing difficulties for management. As one Correctional Manager explained, “The [treatment centre] is not very popular. […] We see people do their careers here, but not for the right reasons.”
Governance is more than just a division of duties and signing authority. The issue of who has signing authority over which sectors with respect to clinical decision-making, while important, pales in comparison to the broader issues of governance. These include staff selection, staff training, onboarding of staff, and a mission or mandate that acts to combine the efforts of all staff toward a common goal. Good governance and leadership in the aforementioned areas set the tone, expectations, standards, goals, and achievement potential of any facility. These, in turn, have impacts on the work environment, staff morale and resilience, and ultimately, on the patient’s quality of life.
6. A Lack of Specialization Required in the Recruitment, Selection, and Training of Staff
The United Nations Standard Minimum Rules for the Treatment of Prisoners: Importance of Recruitment, Selection and Training of Staff in Specialized Facilities
Rule 74:
1. The prison administration shall provide for the careful selection of every grade of the personnel, since it is on their integrity, humanity, professional capacity and personal suitability for the work that the proper administration of prisons depends. […]
Rule 75:
[…] 2. Before entering on duty, all prison staff shall be provided with training tailored to their general and specific duties, which shall be reflective of contemporary evidence-based best practice in penal sciences. Only those candidates who successfully pass the theoretical and practical tests at the end of such training shall be allowed to enter the prison service.
3. The prison administration shall ensure the continuous provision of in service training courses with a view to maintaining and improving the knowledge and professional capacity of its personnel, after entering on duty and during their career.
Rule 76
-
Training referred to in paragraph 2 of rule 75 shall include, at a minimum, training on:
- Relevant national legislation, regulations and policies, as well as applicable international and regional instruments, the provisions of which must guide the work and interactions of prison staff with inmates;
- Rights and duties of prison staff in the exercise of their functions, including respecting the human dignity of all prisoners and the prohibition of certain conduct, in particular torture and other cruel, inhuman or degrading treatment or punishment;
- Security and safety, including the concept of dynamic security, the use of force and instruments of restraint, and the management of violent offenders, with due consideration of preventive and defusing techniques, such as negotiation and mediation;
- First aid, the psychosocial needs of prisoners and the corresponding dynamics in prison settings, as well as social care and assistance, including early detection of mental health issues.
Deficiencies in the Recruitment and Training of Correctional Staff
“The Correctional Training Program just prepares Correctional Officers to be CX-01s. An online PowerPoint does not prepare someone to come work in an environment like this.”
Warden
“There is a significant lack of discipline and the treatment centre’s management doesn’t have any power over correctional officers. Some of them easily get worked up or are inadequate. I understand that comes from inmates, but to treat them like garbage […]”
Chief of Health Services
“Online virtual training simply does not work.”
Warden
“Training standards appear to have gone downhill. There’s too much online training.”
Correctional Manager
While assessments and qualifications to become a Correctional Officer have more or less remained the same over the past several years, senior operational staff interviewed as part of this investigation shared frustration with a perceived decline in both the selection of quality recruits and their level of preparedness following their completion of the Correctional Training Program (CTP), CSC’s training program for incoming Correctional Officers. The CTP is amended to provide Primary Workers and kimisinaw21 with the women-centred training orientation program (WCTOP), due to the unique nature and needs of the institutional population. In contrast, however, staff destined to work at RTCs receive no additional or specialized mental health training to supplement what (little) is taught via CTP. The program comprises three stages, the first two of which, spanning seven to eight weeks, are completed entirely online22. Given the applied, interpersonal, and intense nature that a position at a treatment centre would entail, such an emphasis on theoretical, online instruction denotes a significant deficiency in the training and preparation of staff.
Looking closer at the content and quality of the training, a total of five modules provide information related to working with individuals with mental health concerns, ranging from family violence to suicide and self-injury prevention and responses, to the fundamentals of mental health. Three modules are offered to target officers’ own mental health and share resources and tools available (e.g., Introduction to the Employee Assistance Program and Critical Incident Stress Management). Over the course of the CTP, the amount of training time devoted to addressing officers’ own mental health exceeds the amount of time spent training recruits on working with individuals who may be experiencing mental health issues. Of a 446-hour program, recruits spend approximately 24.75 hours (only 5.6%) on training related to working with individuals with mental health issues, while 25.6 hours are spent on officers’ own mental health. It goes without saying that officer mental health and safety is an important topic to cover in initial training. The method and dosage of training for staff who will be working in a treatment setting, however, is clearly insufficient and sets staff up for a myriad of challenges in how they approach their work, which in turn, has negative cascading impacts on patient care. While recruits receive an overview of legislation covering personal health information, for example, there exists a degree of confusion about what sort of information can be sought from health care and mental health counterparts. This is particularly concerning given the importance of sharing relevant details about the patient’s behaviour, condition, and potential risks which could impact patient and staff safety. Concurrently, new recruits bound for RTCs should have a more thorough understanding of applicable personal health information and privacy legislation to safeguard patient confidentiality.
Promising Practice: Dialectical Behaviour Therapy (DBT) Training at RPC (Prairies)
To bolster the skill sets of new recruits, the RPC in Saskatoon has taken to delivering its own mental health training to new Correctional Officers. Psychologists act as trainers, facilitating a two-day session on Introduction and Coaching to Dialectical Behaviour Therapy (DBT). This evidence-based psychotherapy focuses on teaching skills to patients to effectively manage significant emotions, deal with challenging situations, and improve their relationships. Callouts for participants occur periodically, and staff are supported by institutional management to take remunerated time away from the facility to attend the training session at the Correctional Learning and Development Centre in Saskatoon.
Specialized training, such as DBT, is generally not provided to correctional officers - but should be a mainstay of training for staff at treatment centres. It is needed, not only to develop a skill set pertinent to the patients they are working with but also to enhance their own resilience, prevent trauma and burnout, and improve their understanding of the decisions made to manage and support patients. Notably, the Public Sector Integrity Commissioner’s report referenced earlier also recommended that the CSC develop and provide specific training on an ongoing basis for correctional officers and managers on working in a multidisciplinary environment, such as the RMHC, which serves inmates with mental health issues.
Deficiencies in the Recruitment and Training of Health Care Staff
While significant issues exist in the recruitment, selection, training, and retention of correctional officers, these issues also extend to nursing staff and other health services professionals. This investigation found that the recruitment of both registered nurses (RNs) and registered psychiatric nurses (RPNs) to work in RTCs was a considerable challenge—in some regions more so than in others. Due in part to a general shortage of nurses and a competitive hiring market, with provincial salaries often being more attractive than CSC nursing salaries, both have negative impacts on recruitment for corrections. It was also noted that staffing these mental health units is particularly difficult given the complex needs of their acute patients and highly demanding work. Senior and middle managers commented that nursing coverage is sometimes difficult, particularly as RNs are reluctant to cover for RPNs. This was reflected in the attitude that “a nurse, is a nurse, is a nurse, at the end of the day” and if coverage is needed, there is no reason why an RN could not cover a shift that is normally staffed by an RPN. This management approach was not well received by nurses.
Similar to the deficiencies with the CTP training, the onboarding training process provided to nurses was described as insufficient to equip any new staff member with the confidence needed to execute their roles working with the complex patient profile of an RTC. The onboarding process, while slightly different in duration across sites, often consists of approximately five days of training, primarily online. It includes reviewing Health Services policies, becoming acquainted with the completion of multiple checklist- driven duties, and completing suicide/self-injury prevention training. Typically, a new nurse would then shadow an experienced nurse for approximately six days (e.g., four 12-hour day shifts and two 12-hour evening shifts). Regrettably, as it was explained, a new nurse would not necessarily be trained by the same person for all six days, resulting in redundancies in training experiences and a lack of continuity. Interviewees commented that six days was insufficient, and some new hires expressed a lack of confidence given the unique setting, structure, and mental health needs of the patients. It should be noted that some sites explained that they were looking at assigning a new hire to one mentor for the entire six days of training to provide continuity. Moreover, an onboarding manual was being assembled at one treatment centre to ensure continuity and a fulsome training experience, as well as to serve as a resource following the training experience. Locally, ongoing training was generally limited to required annual medical emergency training, online refresher training for suicide prevention, and instruction on the administration of nursing-related checklists. At some sites, nurses were given a stipend to spend on training experiences outside of CSC to stay in step with practice and licensing requirements.
Recruitment and retention of other mental health (MH) professionals (e.g., social workers, occupational therapists, psychologists, behavioural counsellors) to work in RTCs, while at times challenging (more so for psychologists) did not present the same challenges as with nursing staff; however, concerns were expressed about both the quality and duration of the onboarding process for MH staff overall. Most of these professionals said that they relied on their professional training and standards to guide their work and drew on their past work experience to assist them in adapting to the CSC regimen. One social worker said that they never would have been able to successfully navigate working at CSC had they not had 20 years of experience working in their field.
7. The “Stabilization” of Behavioural Symptoms of Mental Health Appears to be the Overriding Objective of Co-located RTCs
The objective of a patient’s stay at an RTC largely depends on which facility they are admitted to. While some RTCs include a higher proportion of geriatric and infirm patients, likely to serve longer portions of their sentences in this environment, other facilities treat patients dealing with acute symptoms, who will be returned to their parent institution after a period of stabilization. Rather than identifying and treating underlying factors and emphasizing the psychosocial aspect of care, in most cases, the primary role of the RTCs appears to be to provide pharmacological and short-term medical and/or mental health care to stabilize patients, with the goal of integrating them into the mainstream correctional population. Nevertheless, staff at some sites reported that upon discharge from actual treatment within an RTC, patients have waited months to transfer back to the mainstream population. “Parent” institutions from which patients were originally admitted are occasionally reluctant to accept transfers back into their population. This is further complicated by incompatibles23 at parent institutions, and/or resistance from patients wanting to remain at an RTC, all of which can have a detrimental impact on continuity of care.
Despite a clear need and high demand for treatment at these facilities, they are not immune to individuals who manipulate the system to gain admission. For some, time served at an RTC is considered “easier” than a mainstream institution. This, in turn, leads some incarcerated persons wishing to take advantage of this environment, or the vulnerable population it houses, to take action which could warrant admission or lengthen their stay at an RTC, including self-harming and attempting suicide. Correctional staff referred to the ease with which they believe they can identify who they consider to be a “patient” vs. an “inmate” when on a particular unit. As one Correctional Manager explicitly described these dynamics, “You might be prey at [a maximum-security institution] but here, you’re a predator.”
Nevertheless, in the event that treatment centres encounter a patient who is reluctant to return to a parent institution and may in fact self-harm to achieve this, how do staff assess the value of the resistance to determine an appropriate transition process? The investigative team heard from case management staff who, for example, described their apprehension about informing patients of an impending discharge. They described deliberately delaying informing the patients for fear of contending with instances of self- injury, rather than engaging, analyzing, and resolving the resistance. This resistance, and attitude toward returning a patient to an environment like maximum-security following treatment, speaks to the appropriateness of “testing” for success after a stay at an RTC. Given this, it is unsurprising that readmission to RTCs for additional treatment is common. Moreover, this situation also highlights the inability of the CSC to provide a safe and humane environment in maximum-security institutions - anywhere else feels safer.
Table 3: RTC Admissions, Re-admissions, and Discharges by Fiscal Year
| Fiscal Year | Total Admissions | Percent Re-admissions | Total Discharges |
|---|---|---|---|
| 2019-2020 | 829 | 49.6% | 846 |
| 2020-2021 | 765 | 47.2% | 834 |
| 2021-2022 | 922 | 50.3% | 877 |
| 2022-2023 | 1,109 | 50.6% | 1,083 |
| 2023-2024 | 902 | 55.9% | 922 |
| Grand Total | 4,527 | 50.8% | 4,562 |
Source: Data was extracted from CSC Data Warehouse on September 25, 2024, and includes daily RTC admissions and discharges reported through the Offender Health Information System. CSC advised that the higher admissions in FY 2022-23 is attributed to the use of RTC beds for medical isolation, which was required for all new admissions during the pandemic.
Limited Programming and Employment Opportunities
Due to the varied and often comparatively short length of time patients stay at RTCs compared to mainstream institutions, correctional programs, education, and employment opportunities are limited. We heard that employment and vocational opportunities available to patients almost entirely consist of unit-based cleaning, serving meals, and maintenance. As for programming, the Integrated Correctional Program Model (ICPM), for example, first piloted in January 2010, was billed as a revamped approach to correctional programming designed to provide interventions sooner; improve accessibility, relevance and credibility; reduce redundancies in programs; and make the transition to community programming more seamless. As reported by the Office in its 2010-11 Annual Report, the overhaul of the correctional program delivery model was in response to a trend toward shorter sentences, declining day and full parole grant rates, and a more complex offender profile.24 Responsibility to deliver many programs, some of which were uniquely designed for certain segments of the population and notably offered at RTCs, had also shifted from various disciplines, including psychologists and nurses, to Correctional Program Officers (CPOs). Once an internationally renowned sex offender treatment program for example, the RPC’s Clearwater Sex Offender Program, later known as the “Wellspring” program, no longer exists and delivery of such specialized content have been handed over from Health Services staff to Interventions staff under the ICPM umbrella.
The nature of the RTC population is such that run-of-the-mill ICPM programs and education classes cannot be delivered in larger group settings regularly. As previously noted, the existing infrastructure and limitations on space also pose a significant impediment to delivery. An “adapted” version of ICPM can be delivered in smaller group sizes, with simplified language, more repetition, and less content; however, some sites did not have CPOs trained to deliver this version, while others could only offer what few ICPM streams (e.g., multi-target and sex offender streams) are available in an adapted format. Nevertheless, some facilities, such as RPC, reported having the capacity for one-on-one programming for more complex cases, made possible by support from institutional management. The consequence of this is that individuals housed at the RTCs will experience delays in their correctional plans by virtue of some of these realities and limitations. Invariably, a stay at an RTC will unfortunately result in delayed opportunities for early release in many cases. Punishing those who have mental health issues to serve longer periods of incarceration seems grossly unjustified and tantamount to a human rights violation.
Furthermore, despite the fact that Indigenous patients are also significantly overrepresented within RTCs, accounting for 35.9% of the overall RTC population25, the investigation found that cultural programs and services available to Indigenous patients at RTCs is greatly lacking. Sacred grounds were observed to be small, barren, and cramped. Some units were found to be lacking proper ventilation to accommodate indoor smudging ceremonies, leaving those wishing to participate to do so outside in the elements. As a further example, the RPC, which has the highest proportion of Indigenous patients at around 62%26, does not have a four-season sweat lodge. Such limited access to Indigenous programs and services is inconsistent with law and policy.
While “stabilizing” patients’ symptoms with the goal of returning them to a mainstream population may be the foremost goal of the RTCs, it is not uncommon for patients to be released directly back into the community. Given the absence of meaningful employment opportunities or vocational training, these individuals are hardly prepared to enter the workforce. In the absence of dedicated discharge planners, social workers are typically tasked with this as an additional responsibility, despite carrying a caseload of their own. Part of these duties, in conjunction with the patient’s Parole Officer, involves ensuring that the patient is connected with adequate mental health supports, has proper identification, and has sufficient medication to cover this transition. As explained in greater detail in Community’s Burden: The Discontinuity of Post-Release Mental Health Services in this report, this is often not the case and continuity of care into the community is tenuous.
8. Per a Review of NBOIs, CSC has Systematically Failed to Learn from or Prevent Numerous Serious Incidents and Deaths.
When an incident occurs in an institution or in the community, the respective authorities within CSC may convene an investigation or review. According to CSC’s website, the objectives of investigating an incident are to: 1) assess and report on the circumstance surrounding the incident; 2) provide information so that, if required, actions can be taken to prevent similar incidents; 3) learn about and share best practices; and, 4) make findings, and recommendations. For serious incidents (e.g., resulting in serious bodily harm or death), National (Tier I and Tier II) boards of investigation can be convened under various sections of the CCRA, depending on the nature of the incident.
To better understand the circumstances under which serious incidents occur within the RTCs, and furthermore, review how these incidents are investigated, reported on, responded to, and prevented by the Service, this Office conducted a five-year review of National Boards of Investigation (NBOI) into serious incidents at the treatment centres. During this time, a total of 37 NBOIs were conducted further to incidents at each of the five RTCs. The incidents under investigation included: 19 deaths in custody, eight attempted suicides, including three attempted suicides with subsequent self-injury, and four alleged sexual assaults. Other incidents under investigation included incidents of self-injury (2), escape (2), injury (1), and forcible confinement of staff (1). The Regional Psychiatric Centre had the highest number of incidents (16) during the review period.
While each incident involved unique circumstances, the review yielded the following thematic findings:
- Incidents, including preventable deaths of individuals in custody, in-part stem from a disjointed, task-oriented, and reactive work culture. It became evident through reviews of a number of incidents that staff are often working in silos, resulting in a dangerous, and in some cases fatal, breakdown in communication and effective patient care.
- As a consequence of a prevailing task-oriented and reactive work culture, important case information is being documented but not being used to inform action, intervention, or care that could otherwise be consequential in the prevention of serious incidents.
- Conversely but relatedly, poor documentation practices, particularly the insufficient recording of relevant changes in the mental health status of individuals, creates significant informational gaps that could otherwise be used to flag concerning fluctuations or trajectories of decompensation. This information tracking is essential to the prevention of serious incidents and deaths
- As identified in the Office’s previous reporting, numerous incidents across multiple regions were noted to involve security patrols, including formal stand to counts, that were of poor quality due to their duration, frequency, and/or verification of a living, breathing body.
- In addition to poor documentation and sharing of information, incidents denoted a poor understanding and/or interpretation by both operational and health care staff as to signs of distress or behaviour that is clearly abnormal.
Consistent with many of the findings of the 6th Independent Review Committee’s Report, this review yielded several concerning aspects of the NBOIs themselves. Our review found that the NBOI at the RTCs and the resulting reports were:
- Surprisingly silent on important contextual details regarding the quality and nature of interventions and therapy provided to individuals with mental health concerns.
- Overly focused on compliance issues (e.g., completion of tasks in accordance with policy) and proper placement of documentation in an individual’s file, to the exclusion of assessing the quality of treatment or interventions given.
- Lacking attention to investigating, assessing, and offering substantive recommendations on mental health assessment and treatment plans (or lack thereof) for those with mental health concerns; consideration of participation and progress through treatment/intervention; and, how treatment resistance was being managed.
- Not consistently nor meaningfully shared nationally with staff as a learning tool, and therefore, failing to deliver on one of their main, and arguably most important, functions: a post-event teaching and incident-prevention tool.
- Rarely used as a knowledge mobilization tool for offering evidence-based examples of effective preventative methods when engaging with individuals with significant mental health needs, particularly those who are in crisis.
9. The Marked Absence of Dedicated Patient Advocates in RTCs Infringes on Patients’ Rights and Needs.
This Office has long called for the implementation of independent and external patient advocacy services in CSC institutions, most notably following the Royal Assent of Bill C-83 (An Act to amend the Corrections and Conditional Release Act and another Act) on June 21, 2019. The bill introduced new health care provisions into the CCRA, formally recognizing CSC health care staff’s professional autonomy and clinical independence. Section 89.1 requires CSC to provide federally incarcerated individuals access to patient advocacy services to help patients better understand their rights and responsibilities related to health care.
My Office has made such calls in excess of a decade, with recommendations being issued in 2012-13, 2017-18, and most recently in 2022-23. These have included direction for CSC to look to domestic and international best practices in the field of patient advocacy, to develop a strong model to provide patients with advice and support and ensuring their rights are fully understood and respected.
An independent and robust patient advocacy model is necessary in all institutions, but this requirement is only magnified in a treatment centre setting as certain barriers we have previously highlighted disadvantage the most vulnerable. This includes a lack of capacity for informed consent, and, as noted throughout this report, dual loyalties as a result of a correctionally-influenced governance structure. In addition, the Office has previously recommended appointing Patient Advocates to the RTCs as patients can be involuntarily certified, treated, or physically restrained for health care purposes 27.
Six years after Bill C-83 passed and well over a decade since the Office began calling for their creation, there continues to be a lack of action by CSC in implementing independent patient advocates, a pressing need which was evident during the course of this investigation.
Conclusion
As stated in other sections of this Annual Report, the prevalence of mental health issues and the requirement for modern, innovative, tailored, and effective approaches to serving those suffering from mental health issues is more crucial than ever. The aging population within our treatment centres, many of whom have such advanced cognitive and neurodegenerative impairments that any danger to others is null, are sitting idle in what present, ostensibly, as traditional prison environments. External forensic facilities we visited offered a glimpse into what the leading edge of mental health care for offenders can and should look like.
Individuals found to be Not Criminally Responsible do not belong in federal correctional institutions, where their rights and treatment are incongruent with what few RTC-specific policies are in place. Such a practice is as dangerous as it is confusing.
Given the findings stemming from this investigation, including the substandard level of care one would not expect of a designated and accredited psychiatric hospital, the notion that these facilities can maintain these credentials is cause for concern. While CSC may be equipped to provide, at best, intermediate mental health care and temporary services in the event of an emergency, existing facilities are a far cry from external provincial counterparts we visited.
While the RTCs serve an incredibly challenging segment of the institutional population in many ways, a blanket approach to recruitment, selection, training, and deployment have filled these facilities with staff who feel ill-equipped to work with such a population. We encountered numerous dedicated professionals throughout these visits who had the best of intentions and professional dedication, but were bound by prescriptive checklists, a loss of professional autonomy, a culture of muddled governance, and an ever-increasing emphasis on security. This too has led to numerous examples of infighting or tension with health services staff and repeated instances of poor treatment of the most mentally ill individuals in CSC’s custody. For many patients, that very custody should be called into question, as these findings point to a need to re-allocate funding to more capable and specialized provincial and community facilities. While I acknowledge the difficulty in realizing such a shift, exorbitant spending on a single facility will not bring resolution to systemic and organizational issues. If such significant changes are made, however, perhaps the succession of deaths, suicides, and violence can be interrupted. At present, however, these treatment centres are delivering on what would be expected of intermediate care, at best, and are not delivering on providing psychiatric care within a therapeutic milieu.
Before the recommendations below can be addressed, CSC must first action the two recommendations I put forward in my Correctional Investigator’s Message, namely, that RTCs be redefined as Intermediate Mental Health Care Facilities, with emphasis on transferring individuals diagnosed with serious mental illness to community-based psychiatric hospitals better suited to meet their needs; and that the Government of Canada reconsider its recent investment in a replacement facility the Shepody Healing Centre and instead support CSC in reallocating current resources toward facilitating transfers to provincial psychiatric hospitals.
I recommend that once the RTCs are reprofiled as Intermediate Mental Health Care facilities:
- CSC work with mental health professionals to see how the current RTC infrastructure could be significantly improved and become more therapeutic, including the use of paint, plants, grass in yards, benches, carpets, posters, and sofas where security concerns could be mitigated.
CSC's Response: ACCEPTED IN-PRINCIPLE
CSC recognizes that physical environments are key contributing factors that can serve to promote stability, recovery and healing and CSC will endeavor to find opportunities to optimize Regional Treatment Centre (RTC) infrastructure.
RTCs function as therapeutic environments which facilitate treatment interventions, recovery, improved functioning and quality of life. Aligned with the physical design principles of the Health Centre of Excellence (HCoE), as part of the RTC review, CSC will collaborate with internal stakeholders including health and operational staff and managers, and inmates to review the existing infrastructure and physical environments of RTCs with a long-term goal of developing site-specific options to optimize the existing space.
CSC is currently developing a Health Services Action Plan for the Built Environment (HSAPBE), the overarching goal of which is to create a strategic, long-term vision for the facility needs of Health Services across CSC's institutional portfolio. This includes assessing requirements at RTCs and institutional Health Units (including Intermediate Mental Health Units) and understanding how these components will interact and function cohesively to meet the evolving needs of Health Services. This involves examining their current roles, functionality, and identifying opportunities for improvement. A critical step in this process will be developing a comprehensive inventory of existing assets and conducting an analysis of their usage and effectiveness. As a result, updated built environment standards will be developed, leading to infrastructure projects aimed at aligning facilities with these new standards. At the same time, CSC will continue to review projects related to existing RTCs and Intermediate Mental Health Care Units, with a focus on identifying appropriate strategies to create more supportive, therapeutic spaces within these facilities while still meeting security needs. The HSAPBE will provide a comprehensive review of how current and future infrastructure can be significantly improved, the specific projects to achieve physical changes would then have to be submitted into CSC's annual Call Letter Process for prioritization and funding allocations, within budgetary, procurement and contracting authorities and resourcing.
Next Steps:
- CSC has initiated a review of Regional Treatment Centres to provide a standardized baseline of service provision.
- CSC has initiated a review of Health Services infrastructure across CSC's institutional portfolio.
Timeline: Fiscal year 2026-27
- The Minister of Public Safety immediately review and assess release options (e.g., medical and/or geriatric parole) for older and long-serving patients who do not pose undue risk to public safety, and advance legislative amendments to the CCRA, accordingly. CSC should actively invest in community corrections to create bedspace in long-term, hospice and retirement home settings, with a target of 200 beds in five years.
Public Safety's Response: ACCEPTED IN-PRINCIPLE
It is important that the Corrections and Conditional Release Act (CCRA) reflects the needs and realities of the current federal inmate population, including those who are older, require a higher level of medical care, or are approaching end of life. Contingent on their individual risk to public safety, there is a recognition that a federal institution may not always be the most appropriate setting for particular inmates.
The CCRA currently contains provisions that allow for federal inmates to access appropriate medical care in the community through temporary absences. Both escorted and unescorted temporary absences may be authorized for an unlimited period of time if it is for medical reasons. In addition, Section 121(1) provides the Parole Board of Canada (PBC) the ability to grant parole at any time to an offender in exceptional cases, including those who are terminally ill and those whose physical or mental health is likely to suffer serious damage if continued to be held in confinement.
Public Safety Canada is cognizant that older federal inmates and those approaching end of life are a demographic with unique needs and characteristics, and that the services and infrastructure of federal institutions may not always be the most appropriate or sufficient for this population, therefore the Public Safety portfolio will continue to explore ways to strengthen all forms of conditional release.
In addition, as part of CSC Health Services partnership plan, CSC will continue to seek out partnerships focused on post-release services to ensure continuity of care, including working with provinces and territories on barriers to accessing provincial health care faced by offenders upon release, and to explore palliative care options in the community.
- CSC develop a policy specific to the governance and operation of the RTCs, in consultation with external experienced mental health professionals from its inception.
CSC's Response: ACCEPTED IN-PRINCIPLE
CSC acknowledges the importance of role clarity and will ensure that this is reflected in policy and guidelines that are readily available to staff.
As part of CSC's review of Regional Treatment Centres (RTC), CSC will be reviewing existing policy and guidelines related to the RTCs. Amendments to policy will include clear delineation of authorities and accountabilities and policy direction on service provision.
Next Steps: CSC has initiated a review of Regional Treatment Centres to provide a standardized baseline of service provision.
Timeline: Fiscal Year 2026-27
- CSC review the implementation of the Engagement and Intervention Model with a particular focus on its application with those suffering from mental health conditions. CSC should also cease the use of inflammatory sprays as a first response to incidents of self-harm, in favour of health care-driven, de-escalation and therapeutic responses and techniques.
CSC's Response: REJECTED
CSC is committed to managing all interventions, including those involving selfharm, in the safest and most reasonable way possible. Verbal de-escalation and gradual response techniques are prioritized whenever time and circumstances permit. These principles are embedded in CSC's Engagement and Intervention Model (EIM), which promotes health-focused, person-centred responses and continuous assessment of risk. Staff are expected to consider each inmate's individual needs, particularly those related to mental health, and to ensure that interventions are necessary, proportionate, and focused on safety.
In 2021, CSC completed a comprehensive evaluation of the EIM, which led to several recommendations. These have since been implemented to improve the model's effectiveness and ensure it remains responsive to institutional realities.
The EIM is a risk-based framework that guides staff in responding to incidents, including those involving mental health distress. It emphasizes reasonable and health-informed decision-making, with staff required to continuously assess an inmate's mental state, ability to follow direction, and history of self-injury or suicidal behaviour. OC spray is only used when other de-escalation methods have proven ineffective and the situation presents a serious risk.
To further support individuals at risk of suicide or self-injury, CSC has implemented a Clinical Framework for Identification, Management, and Intervention for Offenders with Suicide and Self-Injury Vulnerabilities. This framework promotes proactive, least-restrictive interventions, timely follow-up, and enhanced staff training. It views suicide risk as a continuum requiring different levels of care and encourages early, preventative action. A key component is the Safety Plan-a collaborative and evolving document developed by staff and the inmate to help recognize warning signs and prevent crises.
Next Steps: Ongoing monitoring
- CSC develop a governance model for RTCs, similar to that of external community forensic psychiatric facilities, including an autonomous reporting and governance structure so that all matters related to health, from separate staffing rosters to training of staff, to complete and unfettered control over budgets and resources, are decided by clinicians, not Wardens or operational staff.
CSC's Response: ACCEPTED IN-PART
Correctional Service Canada (CSC) recognizes that clear governance is essential for the effective use of Regional Treatment Centres (RTCs) and for delivering high quality patient care. To support this, CSC has implemented a governance model that clearly defines the roles of both health services and institutional operations.
Since September 2007, CSC has integrated service delivery, line authority, and accountability for health managers under the Health Services Sector. This integration ensures that managers responsible for health care-whether in mainstream institutions, the community, or RTCs-report directly to the Assistant Commissioner of Health Services. Specifically, physical health services in mainstream institutions were integrated in 2007, mental health services in mainstream institutions and the community in 2013, and RTC services in 2014.
This governance structure ensures that staffing, scheduling, and budget management for health services are overseen by health leadership, not operations. While this model is already in place at all RTCs, CSC will update its health policies and guidelines to clarify roles and responsibilities and ensure consistent understanding and application across the organization.
Next Steps: CSC has initiated a review of Regional Treatment Centres to provide a standardized baseline of service provision.
Timeline: Fiscal year 2026-27
- CSC develop training, onboarding, policies, procedures and directives specific to the function and purpose of RTCs and the welfare of patients.
CSC's Response: ACCEPTED
CSC recognizes the importance of clear communication with staff regarding roles and responsibilities, particularly in specialized environments like Regional Treatment Centres (RTCs). To support this, CSC is refining internal processes to better assist staff and ensure consistent understanding across the organization.
As part of its Health Human Resources strategy, CSC is improving onboarding procedures for health services staff. This includes addressing the unique onboarding needs of RTC staff, which will be informed by a learning needs assessment.
In parallel, CSC Health Services is conducting a comprehensive review of professional development needs to ensure health care professionals, including those at RTCs, are supported in working to their full scope of practice.
In addition, CSC will be reviewing existing policies and guidelines related to RTCs to identify areas for clarification and efficiency. Updated policies will clearly outline the function and purpose of RTCs, with a strong focus on the health and well-being of incarcerated individuals.
Next Steps:
- CSC has initiated a review of Regional Treatment Centres to provide a standardized baseline of service provision.
- CSC will refine onboarding procedures for health services staff, as part of the Health Human Resources strategy.
- CSC is conducting a full review of professional development needs to help health care staff work to the full scope of their practice.
Timeline: Fiscal year 2026-27
- CSC develop a specific mandate and mission statement that reflects the purpose, goals, and methodology around which staff across disciplines can collectively unify their efforts to achieve a common goal.
CSC's Response: ACCEPTED
As part of its ongoing review of Regional Treatment Centres (RTCs), CSC will be examining all existing policies and guidelines to establish a standardized baseline for service delivery. This work will provide clear direction on the mandate and mission of RTCs, ensuring alignment with CSC's broader organizational goals.
Following this comprehensive review, CSC will also ensure that relevant performance metrics for RTC activities are incorporated into its performance measurement framework. This will support consistent monitoring and accountability across all RTCs.
Next Steps:
- CSC has initiated a review of Regional Treatment Centres to provide a standardized baseline of service provision.
- CSC will be reviewing all existing policy and guidelines related to the RTCs to provide a standardized baseline of service provision.
Timeline: Fiscal year: 2026-27
- CSC develop practices to ensure that the NBOI process balances investigation of compliance-driven issues with issues of quality, nature, and frequency of interventions provided to individuals with mental health concerns, including treating these reports as consistent, service-wide, learning and knowledge mobilization tools, in order to prevent further deaths and serious injury.
CSC's Response: ACCEPTED IN-PART
A collaborative review process involving the Incident Investigations Branch (IIB), and the Health Services (HS) Sector determines the mechanism based on which a death in custody will be reviewed - i.e., National Board of Investigation (NBOI) or Quality of Care Review (QCR). When a death is initially presumed to be of natural cause, HS proceeds with a convening order to conduct a QCR in accordance with rules, regulations, and the CCRA to assess healthcare-related factors. The impacted site conducts a local care review, and those insights are used to draft a comprehensive national QCR.
If it is determined that a NBOI is required, the review targets key areas specific to the incident, to allow for the identification of recurring issues and best practices for the management and care of all individuals under CSC responsibility. Clearly defined areas of investigation allow for better understanding of issues, which includes the nature and quality of interventions provided to all individuals. To inform decision making and to highlight systemic issues, the collection, analysis, monitoring, and evaluation of data to identify trends will contribute to quality improvement. The information sharing and dissemination of the results from the QCRs and NBOls allows for continued learning and ongoing engagement of all CSC staff to prevent similar incidents from occurring in the future.
Next Steps:
All incidents involving death or serious injury are reviewed weekly to ensure the correct sector is assigned to lead the investigation and to prevent duplication of efforts.
Timeline: Ongoing
Revision and implementation of strategic investigation areas within Convening Orders to focus on key aspects of each incident, streamlining the investigation process.
Timeline: Summer 2025
Results from both the QCR and NBOI processes are shared through multiple means, and along pre-established timeframes.
Local & Regional/National Debriefs: Scheduled at the completion of each NBOI to review and discuss findings and recommendations.
Timeline: Ongoing
National Investigations Meeting (NIM): Senior Management from across the organization meet on a quarterly basis to review and discuss findings on recurring issues and trends, best practices and recommendations/action plans for NBOIs and QCRs.
Timeline: Quarterly
Significant Findings Bulletins: Regular and ongoing publication of Bulletins containing a summary of quarterly findings from NBOls presented at each NIM (4 times/yr) as well as thematic Bulletins on recurring issues and trends (as required but anticipated 4 times/yr).
Timeline: Ongoing
Continued engagement of IIB National Investigators in the Learning Continuum initiative implemented in January 2022. This includes a range of training opportunities designed to prepare investigators to work effectively in a correctional environment. The focus is on conducting impartial investigations and understanding all relevant factors-such as an inmate's social, physical, and mental health history, as well as their vulnerabilities and protective factors.
Timeline: Autumn 2025
CSC is currently updating the QCR process to strengthen care delivery, improve quality assurance and improvement, and enhance collaboration across sectors.
Timeline: Autumn 2025
- CSC immediately introduce, at a minimum, one Patient Advocate in each RTC to support patient-centred care and provide legitimately independent advocacy for patients in navigating the medical system in a correctional context.
CSC's Response: ACCEPTED
CSC Health Services is currently implementing a Patient Advocacy Service (PAS) in 2025. Priority populations for the PAS will include women offenders, maximum men offenders at sites offering intermediate mental health care services and Regional Treatment Centres (RTCs). Consistent with the Corrections and Conditional Release Act (CCRA) the PAS will "support inmates in relation to their health care matters; and assist inmates, their families and/or an individual identified by the inmate as a support person to understand the rights and responsibilities of inmates related to health care".
The PAS model is supported by a Patient Advocate Service Advisory Committee, which launched in Spring 2025, and is comprised of both internal and external stakeholders. The PAS Advisory Committee provides advice and recommendations for the implementation and delivery of the PAS program.
Next Steps: CSC has begun implementing a Patient Advocacy Service (PAS), which includes setting up an Advisory Committee and will eventually expand to offer services in each CSC region.
Timeline: Fiscal year 2025-26
Finally, while only four of the five RTCs are designated psychiatric facilities under provincial health legislation, I am informing the CSC that I will send a copy of this report to the five provincial Ministers of Health where RTCs are located to share my concerns about the provincial designation of RTCs as psychiatric hospitals under their respective provincial mental health legislation.
Appendix A: RTC Use of Force Case Examples
A Collaborative, Interdisciplinary, and Person-Centred Approach to a Post-Use of Force Assessment
On Friday, January 19, 2024, at the RTC (Millhaven), a patient in distress activated his cell alarm. Responding staff found him threatening self-harm if a Correctional Manager (CM) was not called to resolve issues with some of his personal property. The individual climbed on top of his toilet in the observation cell and attempted to dismantle the fire suppression system. A correctional officer gave multiple direct orders for the individual to get off the sink and to stop threatening to self-harm. The individual then leaned forward, leading the officer to believe that the patient was going to jump headfirst onto the concrete floor. The officer subsequently sprayed the patient with oleoresin capsicum (OC) spray, causing the individual to step down to the floor. Despite recommendations from staff, the individual refused to be moved to decontamination. While the actual use of force was not captured on handheld video – making the OCI’s review of the intervention not possible – a Use of Force Analyst reviewed the approach taken by staff after the inflammatory agent was deployed.
Following the use of force, staff engaged with the patient on multiple occasions. Both health care and mental health staff attended the patient’s cell to discuss his mental state and physical wellbeing. The mental health representative discussed options with him for roughly five minutes and offered mental health supports, despite the individual’s agitated state. The patient became increasingly hostile, leading both mental health staff and attending correctional officers to engage in a “wellness first approach.” For example, they were observed encouraging him to accept the decontamination shower to “clear his head.” After the mental health staff left the area, the remaining staff continued to engage with the individual, reassuring him that the CM was on his way while reiterating that a decontamination shower would be good for him. Health care and correctional officers could be heard discussing among themselves a plan to keep the individual safe, agreeing that their ongoing efforts to encourage him to take a decontamination shower were essential. After the individual climbed on top of his toilet once more, staff were observed engaging in conversation in attempts to de-escalate the situation. Once the CM arrived at the cell, he engaged with the individual, asking questions regarding his wellness and physical wellbeing. The patient then provided details as to why his behaviour initially escalated, namely because he wanted an institutional transfer and had an issue with his personal effects. The patient again refused another attempt at convincing him to take a decontamination shower. The continued efforts of staff to encourage the patient to decontaminate were ultimately successful as he agreed to a shower about 30 minutes following the discussion with the CM.
The approach taken during this interdisciplinary intervention at the RTC (Millhaven) is one that is rarely observed by this Office. Each staff member who engaged with the patient spoke in a calm and respectful manner, even in moments when the individual was in an agitated state. They recognized when to engage with him verbally, when to take a step back and give him space, and when to simply inform him that they were present and available to support him. The staff went above and beyond, offering opportunities for decontamination approximately eight times, surpassing what is required by policy. In conclusion, while questioning whether the use of inflammatory agents in the inmate’s situation was the appropriate response, the Office found that once this force was used, it was followed by a “person-centred” approach that should always be prioritized in the particular context of mental health.
Numerous Use of Force Incidents and Questionable Transfer Decisions
In contrast to the first example, the current case demonstrates CSC’s inadequacy in effectively managing individuals with serious mental health needs. This case involves an incarcerated woman with a history of mental health needs serving her first federal sentence who has been involved in multiple incidents, most of which related to assaults on staff, and has been transferred numerous times. Specifically, OCI investigators and analysts identified 66 use of force incidents involving the patient during the period under review (April 2023 – February 2025), amounting to an average of six use of force incidents per month. Analysts noted that nearly half of these incidents occurred in response to self-injurious behaviours, 12 of which occurred at the Regional Psychiatric Centre (RPC), an institution that is supposed to be able to manage mental health needs. There does not appear to be a difference between the interventions taken by officers at RPC and other women’s institutions. In incidents involving self-harm, the same scenario is repeated: initial communication, negotiation, verbal commands, the use of a shield and physical control, the use of a spit mask, the application of handcuffs, and, if perceived to be necessary, leg irons. The offender was then placed in Pinel restraints following authorization from the medical staff. While such a process may seem reassuring at first glance due to its gradual nature, my Office is particularly concerned about the overuse of Pinel restraints, as the frequency of interventions should have provided predictability and led to the consideration of alternatives to such an extreme measure).
Furthermore, since commencing her sentence at RPC in 2023, the offender has been transferred between multiple institutions several times. She has experienced a particularly high number of transfers for such a short period of incarceration and, in some cases, has been in an institution for less than a month before being transferred again. Despite other institutions identifying RPC as the most appropriate institution to address this individual’s needs, she was still transferred multiple times without a clear plan to manage her needs effectively. For example, the reason given by RPC for the decision to transfer her out was, “a general lack of commitment to daily activities, programs and therapy.”
Drawing concerning similarities to cases we’ve previously reported on,28 my Office finds it troubling, to say the least, that after determining a person’s mental health needs to be serious enough to warrant admission to a treatment centre, the Service would cite “a general lack of commitment” by the patient to justify the end of care in a psychiatric facility. However, CSC decided to transfer the patient to an institution where therapeutic personnel and infrastructure are lacking. It should be no surprise if her decompensating behaviours begin to increase, resulting in more use of force incidents. My Office continues to closely monitor the offender’s situation within her institution, particularly with respect to her involvement in use of force incidents, any mental health assessments she may be subject to, as well as any decisions that may impact institutional transfers
Evidence of Violence Against an Incarcerated Person and False Staff Testimony
On March 10, 2025, at the Regional Mental Health Centre, a patient attempted to grab the hand of an officer who was delivering hygienic paper through the cell’s food hatch. Believing that his colleague was at risk of being assaulted, a second officer rushed to the scene and struck the patient’s hands six to seven times through the open hatch. However, no injury was identified by the nurse during the physical assessment. In their reports, the officers involved in the incident justified the blows against the individual by stating that he had managed to grab the first officer’s arm, and this constituted a legitimate threat warranting a use of force response. Our analysis of the incident, however, revealed that the patient’s attempt to grab the officer’s arm was unsuccessful. The first officer in question backed away and was clear of the food hatch before his colleague stepped in to administer the blows. Given that the patient remained confined to his cell and that the blows were inflicted nearly ten seconds after the second officer began intervening, it is impossible that any de-escalation techniques were employed in response to the threat, if ever one was present.
Following the preliminary review, the institution refuted the testimony of the two correctional officers and determined that the use of force was neither necessary nor proportionate. The review also concluded that they did not comply with the rules set out in the Engagement and Intervention Model (EIM), which is supposed to provide guidance to CSC staff in applying a balanced approach to using a person-centred intervention.
In this incident, my Office is not only concerned about the abuse experienced by the patient, but the fact that he is a person with mental health needs makes this abuse all the more abhorrent. Equally shocking is that two public servants (i.e., the Officers who attended the offender’s cell) attempted to cover up a flagrant violation of both the Criminal Code and the rules governing the use of force in federal prisons by providing false testimony in internal reports. CSC’s response to the misconduct of the staff involved in the incident was limited to verbal reminders during debriefing meetings and using the case for training purposes. In this instance, institutional management deemed the situation concerning enough to alert my Office and the police. Therefore, the Office does not believe that such a response is adequate, given the circumstances.
Falling Through the Cracks: Federally Sentenced Individuals with Cognitive Deficits
Cognitive disorders and deficits29 relate to impairments in an individual’s cognitive functions, including learning, memory, perception, attention, problem-solving, language, and executive functioning. Although the severity and range of cognitive needs can vary considerably across individuals from mild to severe, people with cognitive deficits may experience memory loss, challenges with attention, difficulties with organization and planning, and difficulties in language or perceptual abilities.
It is evident across the literature that there is no consistent definition for intellectual and cognitive disorders or disabilities, and terms can vary depending on what one is trying to capture (e.g., formal diagnostic terms vs. broader inclusive terms). For the purpose of this investigation, cognitive deficits will be used as an encompassing term for a range of developmental, cognitive, intellectual, and select neurological disorders and impairments, with a particular focus on issues related to intellectual developmental disorder (IDD), fetal alcohol spectrum disorder (FASD), autism spectrum disorder (ASD), traumatic brain injury (TBI), and some reference to attention-deficit hyperactivity disorder (ADHD).
Cognitive Deficits: Prevalence and Challenges in the Correctional Environment
While most people with cognitive deficits never become involved in the criminal justice system, there is growing evidence to suggest that these individuals are overrepresented in correctional settings30. There is wide discrepancy in the Canadian and international literature regarding prevalence rates due to variability in methodologies, assessment tools, population samples, definitions, etc. For example, prevalence rates for ASD in corrections range from 2% to 17%31 while rates for TBI range from 5.5% to 46%32. Rates for FASD in some countries, such as Australia, are as high as 36%, while in Canada, the prevalence of FASD in correctional settings varies widely based on the method of assessment used, ranging from 1.8% to 23%33. Knowing the prevalence is important for correctional agencies as it provides a sense of scope around individuals’ needs, which should be used to inform the proper allocation of resources, services, and approaches to case management.
Cognitive deficits can lead to potentially challenging behaviours due to impairments in one’s ability to follow rules and directions, regulate emotions and actions, and understand social cues and behaviours. Research suggests that these issues can lead to disadvantages in custodial settings as they may make individuals targets for violence and victimization and can be mistaken for intentional non-compliance by staff, resulting in punitive measures.34 This leads to increased isolation, higher levels of security, disproportionate levels of use of force and an ongoing cycle of problems.35
According to the literature, individuals with cognitive deficits are often confronted with limited resources in corrections, including support mechanisms and adequate programming.36 Persons in custody often experience difficulties with rehabilitation in the institution and in their transition back to the community due to their unique needs and limited resources and services. Research has shown this often results in a feedback loop of recidivism.37As one article so aptly put it, incarcerated individuals with disabilities (including intellectual) are the ‘forgotten prisoners’ and subjecting them to an inherently inadequate, problematic, and ‘ableist’ prison environment and culture “simultaneously overlooks, compounds and further punishes their disability.”38 Although our Office has touched on similar issues, such as learning disabilities in educational contexts in the 2019-2020 Annual Report, cognitive deficits is an area we have not investigated in-depth and, therefore, one that warrants specific attention.
It is important to state that CSC is not the only correctional authority who is not addressing cognitive deficits appropriately. From my experience, I am certain that, universally, all provincial and international correctional authorities have not given sufficient attention to this important issue. A recent landmark report from the Office of the Inspector of Custodial Services from the Government of Western Australia investigated this specific issue, noting multiple gaps and challenges in the management and support of individuals with cognitive deficits in custody.39 In my opinion, this is a unique opportunity for CSC to demonstrate domestic and international leadership by developing evidence-based strategies to address cognitive deficits in a prison setting.
Current Investigation
For the current investigation, the Office conducted a review of CSC’s approach to identifying, supporting, and tailoring services and interventions for individuals with cognitive deficits. As noted above, this investigation focused on FASD, TBI, ASD, and IDD. Although we did not exclude ADHD or learning disabilities,40 they emerged more so when looking at specific areas, such as programs and education. Age- and dementia- related deficits were beyond the scope of the current report given the unique mental and physical health needs of this population. The Office previously published a special report on the aging population in corrections in 2019, which included a focus on cognitive challenges related to individuals with dementia and Alzheimer’s and the inherently problematic issue of corrections acting as long-term care facilities.41 The issues raised in this report still stand today and will continue to become more pronounced as the aging correctional population grows.
We relied on multiple sources, including reviews of international literature,42 CSC documents, policy and data, as well as semi-structured interviews with 35 CSC staff. The staff interviewed varied in positions (e.g., psychologists, chiefs and managers of mental health, education staff, program staff, nurses, social workers, occupational therapists) and included representation from all regions, all security levels, and both men and women’s facilities.
We are very grateful to the Centre for Addiction and Mental Health (CAMH) for the support and expert advice we received over the course of this investigation. CAMH completed a comprehensive literature review for us and several psychiatrists and mental health professionals provided us with valuable information and advice. CSC would greatly benefit from CAMH’s expertise and should consult with CAMH as a partner in its response to our recommendations. CSC should also consider involving the Institut national de psychiatrie légale Philippe-Pinel (INPLPP) in Montréal, Quebec, as it attempts to address the important gaps in services for people with cognitive deficits. INPLPP has also developed significant expertise in this area.
Over the course of this investigation, through the information gleaned from our data analysis, document reviews, and interviews, the following themes emerged:
- Outdated and vague policies provide little guidance.
- Prevalence of cognitive deficits is likely underestimated.
- Stigma, safety, and challenges of institutional living for individuals with cognitive deficits.
- Ineffective and inconsistent screening and assessment tools lead to individuals falling through the cracks.
- Correctional programming, education, and vocational training are lacking responsivity.
- Inadequate staff training and insufficient resources compromise the quality of care.
Findings
Outdated and Vague Policies Provide Little Guidance
The primary policy documents that guide CSC management of federally sentenced individuals with cognitive deficits are the Guideline 800-10: Intellectual Disability 43 and CSC’s Mental Health Guidelines.44 In our review of these documents, we found the content and guidance of both to be vague, high-level, and brief. For example, Guideline 800-10 is specific to intellectual disability, is a mere two pages long, and does not consider other cognitive deficits, despite the complexity of the needs of this population. The majority of the policy redirects staff to several other policies that speak to generic approaches to CSC operations that seldom mention needs specific to individuals with cognitive deficits. During our interviews with staff, we heard that the policy was seen as inadequate and offered little guidance. Staff also noted that, compared to previous versions, CSC’s current Mental Health Guidelines appear “watered down” and, as one staff member put it, “completely overlook the needs of this population.” Although cognitive needs are different from other mental health conditions, such as borderline personality disorder or schizophrenia, cognitive deficits still fall under the broader category of mental health and thus the responsibility of CSC mental health staff. In addition to requiring updated revisions (this Guideline was due for review in 2020 and has yet to be updated), more concrete direction and practical guidance for staff is clearly needed.
Prevalence of Cognitive Deficits is Likely Underestimated
As noted earlier, the prevalence of individuals with cognitive deficits in the federal correctional system is challenging to establish. Based on data provided by CSC, by their estimates and definitions, only 4.1% of the incarcerated population has a cognitive deficit-related diagnosis, a number that jumps to 17% when ADHD is included (Table 1).
Table 1. Prevalence of Federally Incarcerated Individuals with a Cognitive Deficit Diagnosis
| 2021-2022 | 2022-2023 | 2023-2024 | |
|---|---|---|---|
| All cognitive deficit diagnoses | 12.7% | 16.2% | 17.2% |
| Cognitive deficits diagnoses, excluding ADHD | 2.4% | 3.8% | 4.1% |
| By Diagnosis | |||
| Autism Spectrum Disorder | 0.2% | 0.5% | 0.5% |
| Attention-Deficit/Hyperactivity Disorder | 11.1% | 14.0% | 15.0% |
| Intellectual Disability | 1.0% | 1.4% | 1.4% |
| Fetal Alcohol Spectrum Disorder (FASD) | 0.5% | 1.0% | 1.3% |
| Acquired Brain Injury | 0.6% | 1.1% | 1.1% |
Note. The numbers may not add to the overall total as individuals may have more than one diagnosis
CSC data also indicated that only 1.5% of the federally sentenced population has an Offender Management System (OMS) Cognitive Impairment Flag.45 Depending on how cognitive deficits are defined and measured, these numbers vary considerably even within CSC’s own reporting. For example, previous research from CSC estimated 25% of incarcerated men in one region had some level of cognitive deficit, with 15% having multiple deficits or at least one severe deficit.46 Multiple staff we interviewed stated that CSC is underestimating the prevalence, with some guessing numbers are closer to 25%-30%. One staff member stated that, even if prevalence is on the lower end, the needs are so diverse and require significant support, as she noted, “If I have five individuals with autism, that might look small out of the population, but that’s a lot of work and resources to address their needs.”
Stigma, Safety, and Challenges of Institutional Living for Individuals with Cognitive Deficits
Consistent with the individual challenges described in the broader literature, staff who spoke with us provided an overview of the institutional experience of individuals with cognitive deficits. Several staff noted the challenge of individuals not wanting to accept a diagnosis, admit they have a deficit, or accept help from staff due to a range of reasons, including stigma. This can make it very difficult to effectively engage with these individuals, negatively impacting their rehabilitation. Multiple staff also raised concerns for the safety of these individuals, noting that many of them are at a higher risk of being victimized, bullied, and exploited. For example, staff described incidents where individuals with cognitive deficits had accrued significant debts with other incarcerated persons because they did not understand the concept of debt. In other instances, individuals were pressured or manipulated into assaulting others or getting involved in incidents, resulting in charges and incident reports on their record.
We heard that a lot of these individuals often face challenges with sensory overload, emotional regulation and impulse control, memory, following schedules and rules, and engaging in programs or school. Unfortunately, these symptoms are often misinterpreted as ‘disobedience’ and considered as non-compliance, which can escalate into someone being labelled a “problem case,” creating a cycle of adversity. For some, getting a handle on day-to-day tasks (e.g., hygiene, laundry, meal preparation, keeping appointments) can be a significant struggle. Staff shared that while some individuals may do well with the structure and routine of institutional living, this can easily be undone when a person loses some of that support when that structure changes (e.g., transfer to another institution, release into the community).
Ineffective and Inconsistent Screening and Assessment Leads to Individuals Falling through the Cracks
The screening, assessment, and identification of cognitive deficits are an essential first step toward providing tailored care and interventions. According to CSC policy, there is a formal process in place for the assessment of cognitive functioning, as outlined in GL 800-10. This process includes: 1) screening and identification at intake; 2) referrals by the Chief of Mental Health Services for an assessment and potential diagnosis by a specialized psychologist; 3) the production of a detailed report with recommendations for proper care and intervention; and, 4) the activation of a Cognitive Impairment Need flag in the Offender Management system and dissemination of the report to the Case Management Team for consideration in their Correctional Plan.
According to CSC documentation, the main screening tools used by Health Services to examine cognitive functioning and flag for potential follow-up assessment include the following:
- Computerized Mental Health Intake Screening System (CoMHISS) Assessment, which includes the General Ability Measure for Adults (GAMA).47
- Mental Health Need Scale (MHNS), which includes ratings of Overall Mental Health Need and ratings of Mental Health Need in Specific Domains of Functioning.48
- Mental Status Exam, which includes a structured assessment and “snapshot” of current behavioural and cognitive functioning.
Based on the results of these screening tools, if individuals are flagged, they should be referred for further assessment and a potential formal diagnosis through Health Services. However, many staff we spoke with questioned the effectiveness of these screening tools and their ability to flag individuals for further assessment. For example, with the CoMHISS being computerized, voluntary, and requiring specialized training to administer it, its use is inconsistent. At some sites that did not have staff trained on CoMHISS, no incarcerated individuals were being screened. Even staff who administer the tools had little confidence that these measures are doing an adequate job of screening for cognitive deficits. For example, one staff specifically identified that conditions, such as brain injuries, autism spectrum disorder, and FASD, are being missed by the MHNS and similar tools.
Although CSC policy describes a structured and formalized approach to referring and assessing individuals for a formal diagnosis, information shared with our Office suggests otherwise. We heard from staff that, even if the screening tools identify someone, the process of referral and administering cognitive or neuropsychological assessments has several gaps, specifically, significant variability in access, timeliness, and type of cognitive assessments administered. Some sites had psychologists on staff who were qualified to administer certain assessments, while others had to rely on contracting assessments out to a community resource or refer individuals to a CSC Regional Treatment Centre (RTC). Because of this, depending on where the individual is assessed, different diagnostic tools and processes can be used. While a formal diagnosis is not always required for the identification of an individual’s needs, it can be essential for developing effective treatment plans and determining appropriate supports. In some cases, particularly within the community, a diagnosis is necessary to access services.
Most sites identified resourcing as the main challenge to identifying individuals’ needs early, submitting referrals, and obtaining a timely assessment. There is an administrative burden with these assessment tools and there are limited staff qualified to administer them, meaning that mental health staff must prioritize cases with higher needs and acute mental health issues. This was even more evident at the women’s sites, where the majority do not have direct access to resources at an RTC.49 As one Health Services staff member said, “I don’t have the ‘luxury’ of sending women to the RTC for assessment and treatment. I can submit a referral but that means uprooting the individual and at what cost?" Many sites noted that, unless it’s an extreme case or the individual comes into the institution with an existing diagnosis, cognitive deficits are just not considered a priority for assessment and diagnosis. The priority appears to be on crisis management and stabilization of acute mental health needs. As one staff member put it, the focus is on “putting out fires.” To further exacerbate this resource issue, multiple staff noted that psychologists are almost entirely occupied with trying to complete Psychological Risk Assessments (PRAs), an issue we raised in our last annual report.50 As one Health Services staff member stated, “ There is an issue of mental health assessment versus intellectual assessments and CSC is not in the business of doing assessments of intellectual or cognitive capacity and yet this has a direct impact on an incarcerated person’s incarceration, rehabilitation, and release.”
We heard concerns from all of the staff we interviewed that the current screening and assessment process is missing a lot of individuals with cognitive deficits who require support. We repeatedly heard the expression, “falling through cracks” being used by staff, referring to individuals who get lost in the system, have difficulties adjusting to the institutional environment, and inevitably struggle in their path to rehabilitation. As one staff member said in speaking to her frustrations of the inadequacy of CSC’s assessment tools and process for cognitive deficits, “We miss these guys, and this has a direct impact on the person’s incarceration and release success.”
Fetal Alcohol Spectrum Disorder (FASD) Assessment Challenges – Case Example
Our Office became aware of an individual who clearly displayed cognitive challenges but was being denied opportunities (e.g., temporary absences, work releases) on the basis of likely having FASD. For example, in an assessment for decision where CSC denied a request for an escorted temporary absence (ETA), CSC noted the individual likely had FASD and listed multiple symptoms of FASD as justification for the denial (e.g., challenges with self-regulation, poor problem-solving skills). Despite identifying the likelihood of FASD, there was no evidence that CSC had taken steps to get this individual assessed for diagnosis or provided access to appropriate services. After interventions were made by this Office, at the time of writing, this individual was scheduled for a formal FASD assessment. CSC staff acknowledged this would help guide them in understanding and considering this person’s responsivity issues in relation to decisions around work releases and ETAs.
FASD Assessment and Diagnostic Clinic
The assessment process for FASD is resource intensive and can often be challenging due to unknown or missing information regarding prenatal alcohol exposure, medical history, birth records, etc. The CSC FASD Assessment and Diagnostic Clinic, which was first piloted at the Regional Psychiatric Centre (RPC) in 2018-2019, was established to better identify patients with Fetal Alcohol Spectrum Disorder and develop treatment recommendations to facilitate an individual’s rehabilitation and eventual release. The clinic model is now available at RTCs in the Prairie, Atlantic, and Pacific regions. The diagnostic and recommendations process consists of several stages:
- Intake and screening by the Program Coordinator
- Comprehensive psychological evaluation by the neuropsychologist
- Sentinel Facial Features measurement by the lead clinician psychiatrist
- Assessment of life skills and needs by the occupational therapist
- Clinic meeting with attendance by the whole FASD team
- Communication of the diagnosis to the patient by the clinical Coordinator and psychiatrist
- The discharge planning completed by a social worker.
Despite the RPC clinic showing promising practices with several dedicated staff,51 at the time of our interviews, the Office was informed that the clinic was at a standstill due to staffing and contracting issues.
Correctional Programming, Education, and Vocational Training are Lacking Responsivity
Multiple themes emerged in our interviews regarding gaps and challenges in CSC’s approach to correctional programs, education and vocational training. Decades of evidence have long supported that correctional interventions that align with the principles of Risk-Need-Responsivity (RNR) are more effective in reducing an individual’s risk for recidivism.52 The responsivity principle refers to the provision of interventions and programs in a way that is consistent with the learning style and the abilities of an individual. The concept of responsivity is referenced throughout CSC policy, guidelines, and programming materials. Unfortunately, as our findings illustrate, this principle is often overlooked when it comes to individuals with cognitive deficits.
Correctional Programs
Within CSC, there are two main types of programs available: mainstream programs, which are designed for the general population, and adapted programs, which are intended for those who are unable to engage in mainstream options due to “specific responsivity needs including health needs, intellectual and developmental disabilities (cognitive impairments), physical disabilities, or learning disabilities that might significantly impact their functioning.”53
Mainstream. According to CSC, to complete mainstream programming, “an offender should be able to learn and understand new concepts and skills, understand how these concepts apply to their lives (in regard to themselves and those surrounding them) and be able to understand the impact of these new skills on their risk factors. Within the ICPM [Integrated Correctional Program Model], offenders are expected to be able to sit and learn for a two-hour period, without becoming overly agitated, distracted, drowsy or excessively disruptive.”54 This is an unrealistic expectation for many within the correctional population, not just those managing deficits. We heard from programs staff that individuals with cognitive deficits often struggle with comprehension in mainstream programs and this usually manifests in two ways: 1) an individual struggles to keep up in the program, becomes quiet, tries to hide or disengages; or, 2) an individual becomes frustrated and disruptive, and causes problems with other participants. In these cases, staff noted from their experience that the benefits from programming may be limited, and individuals are often labelled as being non-compliant, both of which can have negative and long-term impacts on their correctional plan.
Adapted. The Adapted Program was designed to provide individuals with content similar to what is included in the mainstream but with modifications such as smaller groups (six participants), shorter sessions, modified content to meet responsivity needs and more opportunities for individualized support from the facilitator. While this may appear to be a promising approach on paper, this investigation noted multiple gaps and challenges in practice. Firstly, adapted programs are only available at men’s sites and primarily only offered at RTCs. Furthermore, we discovered that at some RTCs, the adapted program had not been offered for years, leaving multiple institutions and in one case, an entire region without adequate programming options. Staff also remarked that participation in adapted programming is voluntary, and the idea of transferring to an RTC site often discourages individuals from participating. Some noted that, for certain cases, the disruption of the transfer would do more harm than good.
Secondly, the admission criteria to the adapted program stream are quite strict and therefore limiting. Unless an individual presents with significant cognitive deficits and co-morbid needs, they rarely qualify for participation. Multiple interviewees across different sites described a repetitive cycle of having their referrals rejected. One staff member described being so discouraged by this that they no longer saw the point in “putting all the work into referrals,” knowing they would just get rejected. Consequently, according to CSC, there were only 60 enrolments into these programs in 2023-2024. Given CSC’s gross underestimation of the prevalence of persons in custody with cognitive deficits, 60 enrolments (some of whom may not have even completed the program) is well below the number of individuals who could benefit from these types of interventions. Even using CSC’s own prevalence estimates of individuals with cognitive deficits, these enrolments suggest that CSC is only providing adapted programming to approximately 3% of this population. 55
Thirdly, the issue of unrealistic timelines to complete correctional programs, was a concern raised by staff, citing that these pressures go against the entire purpose of interventions. As one Correctional Program Manager noted, “NHQ is just focused on numbers. Doing more one-on-one work is what these guys need, but that won’t give CSC the numbers they want. There is so much more focus on quantity vs. quality now, it wasn’t like that when I started.” Another programs staff member stated, “dragging them along to complete the program to get an ‘attended all sessions’ and no notable gains (since they are not retaining program concepts, let alone applying them to real life situations) is actually doing them a disservice in their correctional plan.”
We heard from staff that, without having an adapted program easily available and accessible, it is up to program facilitators to put in the extra work, adjust materials, provide extra resources and more one-on-one time to help individuals with cognitive deficits and address their responsivity needs. Although CSC references the Motivational Module – Support Stream (MM)56 as an additional mechanism for ‘eligible’ individuals who require support in their program participation, staff rarely raised this as an effective option during our interviews. While MM is sometimes delivered by other program staff, most of the time the onus falls on the program facilitator to provide the support. As one program facilitator noted, “MM is what we’re already doing. It’s not an extra support.” Some facilitators had taken it upon themselves to get external training in cognitive deficits, purchase external resources on the topic and apply this knowledge to adapt the programs themselves; however, some said they’ve been reprimanded for trying to adapt the materials as it can compromise ‘program integrity’. According to a Correctional Program Manager, “CSC does a horrendous job at meeting the requirements to provide accessible programs for individuals with cognitive deficits. So much of it is dependent on the creativity of the facilitator.”
Although CSC highlighted examples of ‘Responsivity Kits’ that are intended to provide strategies and tools for programs staff working with individuals with cognitive deficits, we heard from interviewees that “nobody actually uses them.” Upon review of these materials, the information appears mostly introductory in nature and does not seem sufficient to meaningfully equip facilitators in working with such diverse needs.
We heard during the interviews from multiple staff that overall, CSC is failing to provide a systematic and effective approach to addressing the responsivity needs of individuals with cognitive deficits in programming. Even an internal CSC evaluation57 flagged similar concerns in 2020, noting that the majority of individuals with intellectual disabilities, learning disabilities or brain injuries were not receiving adequate “accommodations, tools, or support to help them participate, despite these needs.” The evaluation also noted that “staff reported having access to limited tools to address offenders’ needs.” A more recent CSC research report58 reviewed a sample of program facilitator casefiles for participants with cognitive impairments or learning disabilities. Although the review showed a variety of accommodations are being used by facilitators, there is no consistent approach or standardized way of tracking this information. The report acknowledged a notable gap in not being able to demonstrate if the accommodations being used effectively meet individuals’ needs. The findings also suggested there is a significant onus on program facilitators to address responsivity factors of participants with cognitive deficits. Although this is, understandably, a part of their role, we heard from our interviews that facilitators are not being provided the adequate support or tools to carry out these responsibilities effectively.
Education and Vocation
For education, CSC offers the Adult Basic Education Adapted Program, which has been adapted for individuals with “specific education needs that cannot be accommodated in the traditional curriculum.”59 Staff spoke of some promising practices and tools, such as the Digital Education Project (DEP),60 reader pens, and the WordQ program.61 We heard of the importance of providing digital literacy and accessible tools, particularly for individuals with cognitive deficits. The DEP and other digital resources were described as being essential in learning and their introduction has made a significant difference for students with cognitive deficits and learning difficulties. Although there has been progress, staff also acknowledged they are still behind when it comes to technology, accessibility, and educational resources. One site mentioned they had only recently set up working computers in the library, while another site had not long been upgraded from floppy disks. Access to modern technology (e.g., tablets) and the internet, an issue this Office has raised several times,62 is still a significant gap in education, not just for individuals with cognitive deficits, but all federally incarcerated persons.
Another theme that emerged was CSC’s inordinate focus on education and grade- level requirements for individuals to move forward in their correctional plans. As several education staff put it, CSC sees Grade 12 as the only way out, regardless of individual needs, cognitive abilities, or whether it is actually beneficial for the person. One education staff noted, “Inmates with cognitive impairments are often parked in the school, trying to get them to complete their education. Everyone gets frustrated but their Correctional Plan states that they must be in school. We are doing them a disservice as some may never be able to complete their education. What we should be doing is preparing them to be independent in the community.”
One staff member provided a case example of an individual with limited education, multiple cognitive deficits, and learning disabilities who struggled in school and in adjusting to the institutional environment. As a result of staff putting in extensive efforts to provide additional accommodations, tools, and one-on-one support, this individual was able to progress in their high school education further than anyone had anticipated. Despite this notable achievement, they were still labelled as non-compliant as they were unable to complete their Grade 12 education. As one education staff member noted, “To productively engage folks [with cognitive impairments], we must give them things that they can handle, peer support, help them transition from school to employment with a job coach. We are not going to educate them or medicate them out of their deficits, but we are obligated to be doing something!”
Although vocational programs and employment opportunities were not discussed in-depth during the interviews, several staff noted the importance of these programs, particularly for individuals with cognitive deficits. Engaging in employment can provide structure and skills that are essential for these individuals upon release. Some staff noted that appropriate employment opportunities were limited for individuals with cognitive deficits. Interviewees also spoke of the importance of an experienced vocational coordinator who can work with an individual’s strengths and capabilities, while noting this is a staffing gap across multiple sites.
Inadequate Staff Training and Insufficient Resources Compromise Quality of Care
The majority of sites acknowledged their staff have not received adequate training to work with individuals with cognitive deficits. In certain cases, staff took the initiative to bring in external experts to provide workshops for employees to increase awareness and understanding of cognitive deficits. Some staff spoke about using their own personal funds to get training outside of CSC. Interviewees described the need for more hands- on, in-person, interactive training from qualified professionals that focuses on learning and applying skills in a correctional environment. This need became even more evident when referring to operational staff. As one interviewee said, “I don’t think most frontline staff know anything about these kinds of [cognitive] needs unless they have a personal connection to it or experience in this area. Most correctional officers have no idea what’s going on – they just think the guy is ‘weird’ and either completely dismiss and ignore him or focus on him too much and misinterpret his behaviours.”
According to CSC, cognitive deficits are part of the mandatory Fundamentals of Mental Health training provided to all correctional recruits. Upon review of these materials, it became very evident that the training is woefully inadequate. Only a handful of slides are dedicated to cognitive deficits with very limited information and significant omissions (e.g., intellectual developmental disorders or autism spectrum disorder). Furthermore, the recommended interventions, such as, “be patient, offer guidance and reassurance, provide clear directions …”, are perfunctory and common sense. Being patient should be a minimum standard for those working with vulnerable populations, particularly in a correctional environment. We also conducted a review of a three-hour training program on cognitive deficits that CSC recently developed for parole officers and found that, despite the materials being more informative and up to date, it was still introductory at best. As one staff member described, “I can’t think of any other job that requires you to take on so much and so many complex cases with so little training.”
Conclusion
Overall, our findings demonstrate that, despite the individual efforts of some staff, CSC is systematically failing individuals with cognitive deficits. Vague policies and guidelines, inadequate screening and assessment, insufficient staff training, and limited opportunities for modified learning and skill acquisition, are all contributing to federally sentenced individuals falling through the cracks. Individuals are being expected to navigate an already challenging system with inequitable means of meeting institutional expectations, much less being adequately prepared to take on the challenges of reintegration. These gaps are emblematic of a system that has forgotten them. As one staff member stated when reflecting on CSC’s approach to interventions and the management of this population, “We [CSC] were once on the cusp of doing great things 10-15 years ago, but we just stayed stagnant, and, in some cases, we even went backwards. How can we be going backwards? Where did we go wrong? Is it policy? Is it funding? Is it staffing? I think it’s all of the above!”
While the individual staff who took the time to speak with us shared many of their concerns, they also shared some practices that could help better support them in their daily work with individuals with cognitive deficits. These approaches included ideas such as:
- the use of interdisciplinary teams to discuss the individual’s needs;
- peer support programs to help with basic skills, note taking, adjustment to the institutional routine, etc.;
- compensatory strategies and visual aids (e.g., visual calendar, colour-coded notes and supplies, shorter appointments, modified routines);
- occupational therapy and psychoeducation services;
- designated units (e.g., formal and informal units to place individuals with cognitive deficits who require more support, to reduce the risk of victimization); and,
- working with external organizations (e.g., FASD Network63) for resources and support both in the institution and in the community.
A concerning narrative that came through in the course of this investigation was CSC’s notion of ‘treating’ individuals with cognitive deficits, particularly those with more severe deficits. Cognitive deficits cannot and should not be ‘fixed’ or ‘treated.’ Rather, one needs to work with individuals based on their needs and provide the tools and skills required for daily living. This is in line with CSC’s mandate to contribute to public safety by assisting individuals to successfully reintegrate into society. We heard multiple times that CSC takes a one-size-fits- all approach, which sets many people up for inevitable failure. As one staff member put it, “What is the ultimate goal? Is it to check a bunch of boxes and meet reporting requirements, or is it to actually support these individuals and give them the skills they need?” The rigidity and emphasis by CSC on meeting linear prescriptive milestones must be revisited in the context of individual needs and in the spirit of responsivity and, ultimately, public safety.
I recommend that CSC, in close partnership with external, community organizations with expertise on cognitive deficits:
- Review and update Guideline 800-10: Intellectual Disability and the Mental Health Guidelines to provide more comprehensive policy and guidelines for the management and supervision of individuals with cognitive deficits by the end of fiscal year 2025-2026. This must be conducted in consultation with institutional staff who deal with these issues on a daily basis.
CSC's Response: ACCEPTED IN-PART
CSC recognizes the unique needs of inmates with cognitive deficits and has implemented services to support staff and inmates in targeted areas including Fetal Alcohol Spectrum. Disorder (FASD) and intellectual disabilities and will continue to explore additional supports and services for this population.
Effective and timely intervention in addressing the mental health needs of federally incarcerated individuals is a priority for the CSC. Mental health service provision is responsive to the specific level of care required. To provide this, CSC has inter-disciplinary teams of health care professionals to provide collaborative services and supports, and interventions to assist individuals in addressing their mental health needs.
CSC continues to seek engagement of internal and external partnerships to support the provision of health interventions, including in addressing cognitive deficits with a focus on dementia. To this end, CSC will commit to review CSC's current policy (Guideline 800-10, Intellectual Disability) with the intent of updating the information regarding intellectual disabilities. Further, as part of CSC's work on Older Persons in Custody (OPIC), Health Services will explore needs related to working with older offenders with dementia.
Both reviews will be conducted in consultation with internal and external stakeholders with a goal of ensuring staff guidelines and processes are reflective of CSC and community practices.
Next Steps:
CSC will undertake a review and update of Guideline 800-10, Intellectual Disability.
Timeline: Fiscal year 2026-27
NCSC will review its geriatric model of care to incorporate needs of OPIC offenders with dementia.
Timeline: Fiscal year 2025-26
- Identify and implement a consistent, comprehensive, timely and standardized approach to the screening and assessment of individuals with cognitive deficits.
CSC's Response: ACCEPTED
CSC acknowledges the importance of robust screening as a key element of the continuum of care and will continue to look for opportunities to optimize our approach to screening and assessment.
As noted in the response to Recommendation 12, effective and timely intervention in addressing the mental health needs of federally incarcerated individuals is a priority for the CSC. CSC is committed to respond to the mental health needs of incarcerated individuals, including those with cognitive deficits.
Accordingly, CSC will conduct a review of the health intake processes, including consideration of enhancements to screening for cognitive deficits to support treatment planning and identifying any required accommodations.
It should be noted that, in 2018, the Regional Psychiatric Centre in Saskatoon, Saskatchewan began the development of a Fetal Alcohol Spectrum Disorder (FASD) Clinic to provide diagnostic, support and education services to inmates. This initiative has since expanded capacity to Pacific and Atlantic. The goal of this project is to identify individuals with FASD who present with a high level of mental health need and make relevant recommendations for treatment, interventions and community supports as needed. The clinics are staffed by interdisciplinary health care professionals using best practice guidelines to conduct FASD screening, diagnostic and functional assessments (including for co-morbid mental illness) and develop recommendations for an individualized treatment and intervention plan. To date, 52 assessments have been conducted for this population.
Next Steps: CSC will conduct a review of health's intake processes, including screening for cognitive deficits.
Timeline: Winter 2026
- Ensure that adapted correctional programming is made available at all sites, that program facilitators receive the appropriate training to deliver adapted programs, and that the threshold for admission to adapted programs be adjusted to allow for more participants.
CSC's Response: ACCEPTED IN-PART
While CSC is committed to ensuring that offenders have access to the programming they require, there is currently no research to suggest that CSC should expand its eligibility criteria for the adapted programs. In fact, previous research on correctional program participation and cognitive deficit has demonstrated that rates of enrollments in correctional programs between offenders in different groups did not differ, and that offenders with cognitive deficits who began correctional programs were as likely to complete them as those without deficits. The study also noted that previous research had found that CSC's programming facilitators were successfully accommodating offenders with mental disorders (Stewart, L.A., Wilton G., & Sapers, J. (2016). Therefore, CSC is not in agreement with reducing the threshold for the eligibility criteria for the adapted programs to allow more participants.
CSC uses a robust screening tool to help Parole Officers and Correctional Program Officers (CPOs) determine whether an offender should be referred to an adapted program. The tool is intentionally comprehensive to ensure only those who truly cannot participate meaningfully in standard programs are referred to the adapted stream. It assesses specific areas to determine how a cognitive or mental health deficit may affect program participation, and whether accommodations can be made within the regular program streams, including support through the Motivational Module Support stream. Referrals to the adapted program are based on solid evidence, such as mental health assessments from qualified professionals or cognitive assessments from health care staff. Offenders with mild to moderate deficits typically do not meet the threshold for adapted programs, as they can still participate meaningfully. These individuals are likely included in the estimated 25% of male offenders with cognitive deficits referenced in the OCI report.
Of note, CPOs are trained to respond to the specific needs of offenders and have the possibility to adapt the material, when needed to address those needs. Tools such as the responsivity kits are available to staff for this purpose. Furthermore, as part of the program revisions to the ICPM, the initial trainings have been streamlined. As a result, beginning May 30, 2025, all Correctional Program Officers (CPOs) who complete their initial training for the Multi-Target or Sex Offender streams will also be trained in the respective adapted program. Therefore, staff will be more equipped with tools to help adapt the ICPM- Multi-Target or Sex Offender programs when working with offenders with cognitive deficits.
While adapted programs are typically delivered in Regional Treatment Centers across the country, there have been exceptions made in the past to deliver the programs at other sites, based on unique circumstances and needs. CSC will send out a reminder to the regions that they can consult with national headquarters should they feel there is a need to install the program at other sites.
Next Steps:
- Streamline initial trainings so that all CPOs who complete their initial training will also be trained in the corresponding adapted program. A memorandum will be issued to the regions confirming the implementation date of the revised initial training.
Timeline: Completed on May 30, 2025 - A reminder to the regions to encourage them to consult with NHQ if there are unique circumstances or needs that warrant delivering the adapted program at sites other than the Regional Treatment Centres.
Timeline: Autumn 2025
- Develop and implement new mandatory training on working with individuals with cognitive deficits in a correctional environment for all staff by 2026-2027. This should include more comprehensive and applied materials for correctional officer training.
CSC's Response: ACCEPTED IN-PART
CSC recognizes the importance of offering training to staff working with individuals with cognitive deficits in a correction environment. To address the need, CSC offers the following training to CSC staff on cognitive deficit:
- Cognitive Disorders and Personality Disorders:
This training helps staff better recognize and respond to cognitive and personality disorders, including conditions like fetal alcohol spectrum disorder and traumatic brain injury. The training improves understanding of the challenges individuals with these disorders may face and provides practical strategies to support them effectively. The training was offered to Parole Officers in 2024-25 as part of the Parole Officer Continuous Development. - Fundamentals of Mental Health (FMH):
FMH training is designed to give staff a strong foundation in understanding mental health issues commonly seen in correctional settings. It helps staff recognize signs of mental illness, understand how mental health affects behavior, and learn effective ways to support individuals experiencing mental health challenges. The training also promotes respectful, informed, and safe interactions between staff and inmates. This training is mandatory for Correctional Officers, Primary Workers, Correctional Managers, and Older Sisters/Older Brothers. - Awareness of Learning Disabilities Among Offenders: This is offered to all correctional officers in stage 1 of the Correctional Officer Training Program (CTP). This training raises awareness about learning disabilities among offenders and helps staff recognize signs of learning challenges and better understand how these disabilities can affect behaviour and communication. It also offers practical strategies to support individuals with learning disabilities more effectively in correctional settings.
- Various scenarios provided in the Correctional Training Program (CTP): As part of the CTP, staff are exposed to a variety of real-life scenarios to help them recognize and respond to mental health and cognitive challenges. These include situations involving individuals experiencing panic attacks, anxiety, bipolar disorder, fetal alcohol spectrum disorder (FASD), and traumatic brain injury. The training also includes scenarios involving older individuals in custody, such as those living with Alzheimer's disease. These examples help staff build practical skills and confidence in managing complex cases with empathy, safety, and professionalism.
Consistent with the Older Person in Custody Policy Framework, CSC is implementing a geriatric model of care that emphasizes assessment, prevention, intervention, and health promotion. This model is designed to meet the evolving health needs of older individuals in custody, including those living with dementia.
As referenced in the response to Recommendation #12, CSC is actively exploring training needs related to working with older offenders who have dementia. Collaborative efforts are underway to review and expand ongoing training, with a focus on interprofessional education in geriatric care planning and facilitation. These initiatives aim to ensure staff are equipped with the knowledge and tools needed to provide compassionate, informed, and effective care.
Next Steps:
- CSC will continue to offer training on cognitive deficits to CSC staff.
Timeline: Ongoing
- CSC will offer Fundamentals of Mental Health to all new CSC employees.
Timeline: Timeline: Spring 2026
- HS will review its geriatric model of care to incorporate needs of OPIC offenders with dementia.
Timeline: Fiscal year 2025-26
Community’s Burden: The Discontinuity of Post-Release Mental Health Services
“There’s a thought that when they get out of the institution, they’re finishing the sentence. They think, ‘Oh, the community will figure it out,’ but they’re not helping us figure it out! This is where the rubber hits the road, where so much damage can occur. We’re the poor cousin. It’s incredible what we’re able to accomplish with what we have. There needs to be a mind shift in terms of putting a focus on the community.”
CSC Community Staff Member
Compared to other people in Canada, federally sentenced persons enter the correctional system with disproportionately high rates of housing and financial instability64, poor employment and economic outcomes65, low education and literacy66, childhood trauma67, and a high prevalence of mental disorders 68 and cognitive deficits. Add to this the intersection of race, gender, or the stigma of having a criminal record, and it should be no surprise that sentenced individuals face tremendous barriers to reintegration, including access to mental health care.
When a person is sentenced to federal custody, they lose access to provincial health care benefits and social assistance for the period of their incarceration. This ineligibility is based on the premise that the state covers their essential needs while in custody. The Service has a legal obligation to provide every inmate with “essential health care” and “reasonable access to non-essential health care.”69 This obligation is only extended to inmates, not offenders under community supervision.70 As a result, CSC’s delivery of health care can be scaled back considerably at release. Once in the community, there is an urgency to transition responsibility for the individual back to the provincial or territorial health authority. Consequently, the transition from institutional to community mental health services can be delayed or derailed by the change in responsibility over health services, sometimes with devastating effects.
To support this transition and reintegration efforts more generally, CSC is responsible for release planning and community supervision, which includes facilitating a continuum of mental health services. This begins in custody with clinical discharge planning and continues in the community through transitional services offered by CSC’s community mental health teams and external partners.
It is important to acknowledge that access to mental health services in Canada varies significantly across provinces, with rural, remote, northern, and First Nations communities facing considerable barriers to care and social support programs. This poses real challenges for CSC. However, CSC has a statutory obligation to provide health and mental health care services consistent with “professionally accepted standards.”71 Unfortunately, not all communities meet these standards – especially rural, remote, northern, and First Nations – and this disparity can worsen health inequities for individuals under federal sentence. Therefore, if CSC wishes to contribute to public safety through its reintegration efforts, it must take more of an active and coordinated role in addressing these gaps.
From Discharge Planning to Community Mental Health
CSC describes clinical discharge planning as an interdisciplinary and patient-centred process “of identifying and preparing for an individual’s anticipated health care needs after they are released to the community”72 with the goal of ensuring a continuity of care. Discharge planning 73 is led by one or more designated health care professionals and should include the following:
- Confirming the individual has identification, such as a birth certificate, prior to release.
- Ensuring the individual’s medications are reconciled and available on release.
- Collaborating with community partners to share pertinent health information and coordinate follow-up services/appointments to ensure continuity.
- Providing a discharge package that includes prescriptions, health information, a list of referrals, community service providers, and appointment dates.
While discharge planning is provided to all individuals being released from prison health care services to the community, “enhanced discharge planning” is required for those with moderate to high levels of need, including mental health needs. This involves a more in-depth assessment, planning, and coordination process. Once discharged, individuals with moderate to high levels of mental health needs may be eligible for CSC’s Community Mental Health (CMH) services, which may include advocacy, clinical accompaniment, and managing mental health symptoms. These services are prioritized based on risk considerations and Parole Board of Canada imposed special conditions (e.g., participate in treatment or counselling).
While the above continuum is now a key component of CSC’s current mental health strategy 74, it has been two decades in the making. In 2004, this Office reported, “an urgent need for liaison between CSC and community organizations so that continuity of treatment and support will be extended to offenders on release.”75 Shortly after in 2006, the Standing Senate Committee on Social Affairs, Science and Technology published a report, titled, “Out of the Shadows at Last – Transforming Mental Health, Mental Illness and Addiction Services in Canada” (also known as The Kirby Report), which recommended that CSC “establish a case management system that ensures that offenders have access to appropriate mental health treatment upon their release […]”. These reports gave impetus to CSC’s Community Mental Health Initiative (CMHI), which received $29.1 million in 2005 for its first five years. This money would help the CMHI increase discharge planning and allocate resources to community supports and services, including clinical social workers, mental health nurses, halfway houses, and other community partners. In November 2008, CSC published a formal evaluation of the CMHI.76 They found that the initiative “resulted in increased access to mental health services” and the individuals who received these services “were less likely to be suspended or revoked than the comparison group who did not receive CMHI services.” Incidentally, the recommendations issued in this evaluation foreshadowed the findings of our current investigation.
Today, the continuum of mental health care – from clinical discharge planning to community mental health services – is governed by a labyrinth of policies, guidelines, tools, and checklists. Despite this extensive policy infrastructure, this investigation into discharge planning and the continuity of mental health services revealed numerous implementation failures. Our key findings are as follows:
- The overall erosion of CSC’s Community Mental Health services.
- A disconnect between policy and practice.
- Flawed mental health assessment excludes many who need community support.
- Poor engagement and information sharing between institutions and the community.
- Barriers to accessing mental health services on release.
- Significant impediments to accessing housing.
These issues can and have had negative impacts on public safety. CSC is failing Canadians by not providing adequate clinical discharge planning and Community Mental Health services that would ensure the health and safety of federally sentenced individuals, CSC staff, and the public.
Current Investigation
The purpose of this investigation was to examine the continuity of mental health services for federally sentenced persons assessed by CSC as requiring enhanced discharge planning due to high mental health needs. In addition to reviewing CSC documentation, semi-structured interviews were conducted with institutional and community CSC staff, parolees and incarcerated individuals, and external stakeholders. A total of 147 individuals were interviewed across all five regions, representing multiple correctional facilities, parole districts, community correctional centres (CCCs), and over a dozen community-based residential facilities (halfway houses).
Findings
The Overall Erosion of CSC’s Community Mental Health Services
While CSC’s CMH services were impacted by the global pandemic, their erosion dates to well before this time. During interviews, veteran CSC staff often raised concerns, unprompted, about the strain on CMH services, noting a gradual yet noticeable decline in funding and organizational prioritization, beginning shortly after 2010 (i.e., after the initial five- year implementation period). Although total spending on the CMHI and other community mental health services had remained relatively stable since its first year of full funding in 2007-2008, we found a 39% decrease from $13.8M in 2009-2010 to $8.4M in 2024-2025 when adjusted for inflation77. During the same period, CSC’s overall annual expenditures have been relatively stable, keeping up with inflation.78 However, its corporate focus remains on institutional corrections; despite accounting for roughly 40% of the federally sentenced population in 2024-2025 (8,713 out of 23,516),79 Community Corrections received just 12% of CSC’s $3.2 billion budget and 9% of its staff.80 Moreover, less than half of the Community Corrections budget was dedicated to community-based residential facilities, CCCs, and Health Services – a small fraction of CSC’s total budget, which represents a notable underinvestment in community mental health and transitional services.
While investment into CMH has not kept up with rising costs, the changing profile of federal parolees is putting greater demands on community staff and partners to respond to complex mental disorders and addictions. The frustration with having to “do more with less” was evident during interviews. “Community Mental Health needs more resources,” explained a CCC staff member, “more and more guys coming out who need it – we’re basically doing more with less. If somebody retires or quits, they’re just not filling it. They’re clawing it back!” A CMH staff member had this to say, “On paper, the continuity of care is great. In practice, however, it seems that the continuity of care is not a priority. It’s been put on the back burner.”
Though CSC has committed the next two years to reviewing, “the provision of community health services in an effort to establish standardized care,”81 the staff we interviewed expressed misgivings about the future of Community Mental Health.
Disconnect between Policy and Practice
Interviewees universally supported the necessity of providing services upon release to individuals with mental health needs. Those familiar with CSC’s discharge planning policies and guidelines recognized its potential and value but argued that the maze of policies and procedures has actually created barriers to the continuity of care. They shared their frustration with changes to national policies, strategies, and guidelines that are far removed from the reality of community corrections. Given this disconnect, we learned that many staff are unable to keep up with policy changes.
Many interviewees were unaware of the Health Status at Discharge: Gist Report (Form 1371) – a key tool for health and case management staff on health information related to release – or the updated Intake, Transfer and Discharge Planning Guidelines (January 2024). Almost none were familiar with the Discharge Planning Matrix, a quick reference document for staff involved in discharge planning. Many shared that they are so overwhelmed with assessments, checklists, and guidelines that to be in full compliance would hinder their ability to do meaningful work with the individuals they are meant to support. We also heard that there is little if any accountability to ensure that those who need discharge plans are receiving them, or that discharge timelines are being met. As one CSC community staff member put it, “Though we know we’re non-compliant, nobody respects the process […]. The process is so horrible that we’re not able to do the good work we need to do, so we ignore it.”
One assurance of accountability is through the designation of a Discharge Planner. According to CSC’s discharge planning guidelines,82 each institution is expected to assign a “designated health care professional(s) to lead discharge planning for each individual being released,” which includes enhanced discharging planning. Interviewees, however, reported that enhanced discharge planning is often imposed on health staff who are not solely dedicated to this work. As one institutional staff noted, “I think that discharge planning is intense and should be connected to correctional timelines, rather than something done on the side of one’s desk.” CSC confirmed that there are only four funded Discharge Planners across Canada. Unsurprisingly, interviews revealed a less than perfect system, with staff troubleshooting their way through practical barriers and responsibilities beyond their scope of practice. One interviewee experienced in discharge planning spoke about how the role is better suited to social work, rather than nursing – a point that was echoed by many interviewees, “There is a need for better capacity building and partnership building. There’s an assumption that the community has this network but, really, capacity building and partnership building is a long-term endeavour. That’s the role of the social worker, and I think it’s been lost along the way. […] CSC needs to take a good look at this role and how it has changed it to directly impact reintegration.”
There are clearly significant obstacles within CSC’s discharge planning process, including a disconnect between national policies and frontline realities, limited accountability, and a scarcity of designated Discharge Planners. Understandably, staff are frustrated, feeling that their best efforts are undermined by systemic issues beyond their control.
Flawed Mental Health Assessment Excludes Many Who Need Community Support
Beyond the disconnect between policy and practice, there are significant gaps in CSC’s use of mental health assessment tools; measures that are meant to be foundational in identifying a person’s needs and informing treatment planning and case management. In order to assess a person’s overall level of mental health need in federal corrections, CSC has developed its own Mental Health Need Scale (MHNS).83 AAlthough part of a broader mental health assessment process, this scale is the primary tool used to help institutional staff make referrals to the appropriate service or level of care (e.g., self-care, primary, Intermediate Mental Health Care, psychiatric hospital, CMH services). According to CSC, to be eligible for enhanced clinical discharge planning and CMH services, an individual must meet the threshold of “considerable” to “acute/severe” on the MHNS.
During interviews with health and case management staff – both in institutions and the community – we learned that the MHNS falls short in many respects. First, institutional staff explained that it is difficult to meet the threshold for enhanced discharge planning and the data confirms this. Only 5.8% of all federal releases met the threshold in 2023- 2024 (see Appendix B).84 Of these, 13.5% did not have an identified enhanced discharge plan, which means that not all who qualify for enhanced planning and CMH actually receive these services.
Overall, these numbers are incongruous with the level of mental health need encountered by staff, and this is substantiated by CSC’s own data. For example, 45% of individuals referred to Intermediate Mental Health Care85 in custody “did not meet the criteria of considerable or higher mental health need” on the MHNS, which by policy is required for referral to this level of care.86 This suggests that staff are conducting their own assessment of needs, separate from the MHNS, to determine the level of care in a large proportion of cases. Furthermore, CSC’s prevalence research estimates that 12.4% of men87 and 16.3% of women88 are admitted with a “major mental illness” (i.e., major depressive disorder, bipolar disorder, or any psychotic disorder). Together, this data strongly suggests that the MHNS is poorly calibrated to assess a person’s need for mental health interventions,89 especially in the community. As one CMH staff member put it, “The MHNS is being used poorly and incorrectly. […] It doesn’t reflect the actual number of individuals who need enhanced discharge planning.”
Seeing how difficult it is to meet the threshold for enhanced discharge planning and CMH services, it was unsurprising to hear that some well-meaning staff resorted to “massaging” the MHNS to obtain services for their clients/patients. What was surprising, however, was how easily the scale can be manipulated to increase (or decrease) the level of need.
This leads to the second shortcoming of the MHNS: it only focuses on immediate and acute needs. Staff frequently shared how mental health interventions are flagged for individuals who are in crisis or whose behaviours present problems for staff and others. We often heard the adage: “The squeaky wheel gets the oil.” If the person keeps to themselves, they may not be flagged for a mental health assessment or intervention, and it is unlikely they will be referred for enhanced discharge planning. Interviewees also maintained that, even when they occur, mental health assessments are not timely. While the requirement for mental health assessments at intake was adopted into policy on November 30, 2019, with Interim Policy Bulletin 651; compliance remains an issue. Consequently, people with mental health needs are being released from federal custody without being properly assessed and without tailored plans, leaving community partners scrambling for last-minute solutions.
The third and, arguably, the most significant problem with the MHNS is that it was not designed with the community in mind. Section 87(b) of the CCRA requires CSC to “take into consideration an offender’s state of health and health care needs” in preparation for release and community supervision. Several experienced CMH staff explained how the MHNS only focuses on mental health needs in the prison context and ignores the impact of social determinants of health, which can lead to mental health decompensation in the community. As one CMH worker put it: “The guy can be very stable in the institution because they have access to housing, income, a source of prescriptions, but they don’t have these in the community. [The MHNS] is a scale that measures if the person can be in the general population [in custody] to receive primary care or needs another level of care. But in the community, the needs are different.”
For these reasons – i.e., its arbitrary threshold, subjective application, sole focus on acute needs, and disregard for the realities in the community – the MHNS appears problematic as a tool for gauging mental health needs in the community.
Poor Engagement and Information Sharing between Institutions and the Community
In a memo dated May 4, 2015,90 CSC recognized “challenges with the information sharing process between Health Care staff and parole officers.” The memo reminded staff about the importance of information sharing during case preparation and pre-release, “as it directly contributes to the safe transition of offenders in the community.” To better define roles and responsibilities, enhance efforts to communicate, and coordinate the sharing of information, the memo introduced the Discharge Planning Matrix Tool as a solution to be used in combination with the Gist Report. In practice, however, this investigation found communication between penitentiaries and community partners (CSC staff and others) to be inconsistent and inadequate.
We heard that the level of detail provided to community staff through discharge documents, such as the Gist Report, is insufficient to ensure effective continuity of care. As one community staff stated, “the Gist Report from the institution serves a limited purpose as it often doesn’t include the information that we [in the community] need” such as details about medications, diagnoses, appointments, and referrals to community services. Our investigation found that the following factors were the main barriers to information sharing between sectors:
- Health information is heavily guarded, even when it is clearly related to risk (e.g., mental health diagnoses, prescription information, participation in harm reduction programs) and ethical standards are upheld (e.g., “the need to know,” informed and voluntary consent)91. This is exacerbated when case management staff and Health Services work in silos, which is common.92
- Roles, responsibilities, and expectations pertaining to enhanced discharge planning are unclear or poorly reinforced, which leads to critical tasks not being completed.
- Timely and proactive enhanced discharge planning at the institution is uncommon, which leaves community partners with little time to prepare before release or to be meaningfully involved.
One CSC community staff voiced their frustration over the institution’s lack of proactive planning and information sharing, stating, “As a community employee working in an institution, I saw how many [staff] don’t see beyond the walls of the institution. It’s a tennis match where the ball is sent to the community court to deal with. There is an institutional assumption that the community can handle it all, that they will figure it out, that they have resources. Yet, they have no time to plan or to make plans – they react to the lack of planning.”
We learned from community staff that the quality of discharge information and planning improves significantly when there is a robust working relationship between the releasing institution, community parole, and CMH services – especially when a dedicated Discharge Planner and community Mental Health Nurse are involved. Discharge planners should maintain active ties to community resources and possess a strong understanding of the determinants of health. The flow of information between institutional and community staff hinges, to some extent, on obtaining informed and voluntary consent from incarcerated individuals prior to release. We also observed that where mechanisms exist for advanced case planning through case conferences (e.g., monthly or quarterly meetings to discuss individuals with high mental health needs), the opportunity for enhanced information sharing and successful reintegration is improved. This is especially true when stakeholders beyond parole and CMH services are included in planning. For example, non-profits who manage Community-Based Residential Facilities (CRFs) are more willing to accept parolees if they are engaged earlier in release planning. Some non-profits have taken the initiative to create their own in-reach worker positions, tasked with meeting incarcerated persons and advance release planning. Interviewees also emphasized the importance of including the parolee, staff from Community Correctional Centers (CCCs), and institutional staff familiar with the parolee. Together, these strategies help to minimize points of friction, facilitate the flow of critical information, and ensure a continuity of care.
Barriers to Accessing Mental Health Services on Release
As mentioned previously, when a person is sentenced to federal custody, they are no longer eligible for provincial health care benefits or social assistance for the period of their incarceration. This ineligibility is based on the premise that the federal government covers their essential needs while under CSC’s custody. Section 87(b) of the CCRA requires CSC to consider health factors in preparing for release and supervision. Moreover, CSC’s guidelines provide for some allowances related to the provision of health services “on an interim basis” at CCCs and parole offices. 93 However, in practice, interviewees frequently noted how CSC’s mental health service ends abruptly at the prison gates. Here is how one individual under community supervision described his experience: “I’m not aware of any mental health or release plans. I was told that I would be going to the halfway house and that’s it. I have schizophrenia, which is controlled through meds. When I was being released, my meds weren’t set up. […] Didn’t have someone to speak to when released. I felt all alone. I had some parole conditions for mental health. I saw psychology in jail and a social worker. When I was released, those services were stopped […] when CSC doesn’t set up services it has a huge impact on our release. The community can’t prioritize us, and CSC seems to just cease responsibility for us.”
Access to community health care depends on resources that are not always available to parolees since government programs and benefits require a social insurance number and proof of identity. Moreover, a parolee’s eligibility for social or income assistance varies greatly depending on the province and whether they are living in a CRF or a CCC.94 Similarly, drug benefits are included in all health care programs, but coverage is limited and extended pharmacare programs are mostly income-based. Therefore, tax returns must be completed and kept up to date.
Navigating these complexities is challenging enough as it is. At the very least, to access government-funded health and mental health care in the community – including psychiatric and psychological services, medication, and other supports – a health card is required, but unavailable to those in federal custody. To obtain a health card upon release, CSC must ensure that individuals have proof of identity before the release date. This would simplify the process and ease the burden carried by community staff and partners.
The issue of missing identification and health cards has been deliberated by CSC and its stakeholders ad nauseum for decades. It was raised by CSC Evaluation in 201795 and again in the Auditor General’s 2018 Fall report where it said that CSC “…often released offenders without a health card.” In response, CSC committed to assisting “offenders in obtaining personal identification (ID) prior to release” and “to improve collaboration with provincial and territorial health authorities with the objective of removing barriers to accessing health care cards.” However, progress in collaborative partnerships has been minimal, and CSC continues to release individuals without proper identification, an issue that was confirmed by all interviewees. For example, of the 761 releases between 2022 and 2024 where the individual met the threshold of “considerable” to “acute/severe” mental health need, more than half (52.4%) had no health card, an unknown health card status, or requested one but did not receive a health card upon release (see Appendix B).96 One third (33.5%) of the total releases had no health card whatsoever.97 It should come as no surprise to CSC that individuals who deal with financial instability, housing insecurity,98 and live with mental health needs face challenges in obtaining personal identification, and require significantly more support to do so. As one CSC community staff member explained, “Putting onus on the client is unfair. There are so many responsivity barriers to them preparing and submitting applications.”
In the Pacific Region, staff praised the efforts of a regional “ID Coordinator” who did this work for all releases in the region, but over the course of this investigation, this program was discontinued by NHQ. The lack of proper health documentation and health care coverage in the community has obvious negative impacts on sentenced individuals. Without coverage, CSC’s community staff find themselves in the unfortunate position of having to ask external partners to do work for free, with rare exceptions. “We asked them to please send guys with IDs and birth certificates,” said one CRF staff member, “It takes a while to do it in the community and it’s costly. Agencies eat the cost.”
We often observed community staff proactively forming partnerships with organizations that assist with identification, health card renewals, and taxes. Community partners, including parole, have offered “accompaniment” to those who need help getting to appointments due to physical, mental, or financial reasons. One organization spends over $100 a month in mileage costs to offer this service. These expenses are not reimbursed or covered by CSC.
These efforts are crucial, as parolees with mental health challenges face unexpected expenses when lacking health or disability coverage and employment assistance. However, even if the individual successfully obtains an ID and health card upon release, this does not guarantee that they will receive benefits in time or that service providers will accept them. As one staff member put it, “A lot of our community partners get exhausted by our clients. They’ll just refuse to take our clients if it’s not working well.” As a stopgap measure, CSC must provide transitional support to ensure the continuity of mental health services. This support involves covering the cost of bus passes, accompaniment, processing and appointment fees, and food. Though some financial support is available to women through the Women Offender Sector, CSC offers minimal compensation to community staff and partners for federally sentenced men.
Ensuring personal identification is obtained prior to release and offering transitional services would help to remove barriers to community-based health care and social services. It would also reduce the financial burden on CSC’s community staff and external partners who are already overstretched and underfunded.
Significant Impediments to Accessing Housing
“Whereas national goals, timelines and initiatives relating to housing and homelessness are essential to improving the quality of life of the people of Canada, particularly persons in greatest need […]”
National Housing Strategy Act (2019)
The adverse effects of housing instability on mental health and wellbeing have been well documented.99Combined with the pressures faced by justice-involved individuals – especially those under community supervision who struggle to find employment, accessing health services, and overcoming the stigmas associated with a criminal record – housing instability can seriously aggravate mental health issues, increasing the risk of suspensions. As one CSC staff member in the community put it: “If I was a person with mental health issues and didn’t have housing, I don’t know how I’d succeed in the community or comply with my conditions.”
Canada is challenged with rising housing costs and increasing rates of homelessness. One CRF manager explained that, prior to the pandemic, residents were staying at halfway houses between 60 and 80 days, “but now they’re staying 200+ days on average because of the housing crisis – they need a place to stay!” If the individual is past day parole and on statutory release without a residency condition, CSC can temporarily pay for voluntary residency within tight timelines. As a result, CRFs are receiving more voluntary admissions. However, some CRFs can refuse individuals with mental health issues, which is why many end up at CCCs as they cannot refuse anyone who legally requires a bed. Consequently, their clients are often individuals with higher risk and need profiles, and CCCs frequently operate at full capacity with extensive waitlists. For fiscal year 2024-2025, the occupancy for CCCs was 103%. 100
Occupied Rooms at Community Correctional Centres
Given this situation, staff are increasingly left with few options but referring individuals to shelters, though they are reluctant to put persons under their supervision into housing situations that aggravate mental illness or put them at risk of harm or reoffending. One district office developed a “housing committee,” a cohort of staff who volunteer their time to connect with property owners to arrange housing options through social welfare programs. Another organization secured two provincially funded beds that can be used as a stopgap measure for residency or to prevent homelessness when a person’s sentence ends. Despite the best efforts of many CSC staff, parolees with determinate sentences do eventually reach their Warrant Expiry Date (WED), leaving some to contend with shelters or homelessness. As one CCC staff member put it, “We’re releasing them to the street at WED in a tent! We’re trying to help them get housing, but there are over 2,000 people on the community waitlist and our clients are at the very bottom given their criminal history, substance use issues – they’re not ideal candidates. If we fill up here [at the CCC], we can’t keep the voluntary guys anymore, and our guys with medical needs… well, we don’t want to put them out on the street.”
Though our Office is encouraged by Public Safety Canada’s “Federal Framework to Reduce Recidivism Implementation Plan” (2023), which includes initiatives aimed at preventing and reducing homelessness “for individuals that are involved in the criminal justice sector,” the urgency of this issue cannot be overstated.
Conclusion
Inadequate mental health support for federally incarcerated persons not only undermines their successful reintegration—it actively jeopardizes public safety. The underfunding and dysfunction of national policies, coupled with inadequate assessment tools and poor coordination between institutions and the community, leave individuals without essential mental health and addictions care upon release. Financial and administrative hurdles, alongside a severe shortage of housing, further destabilize those already at risk of recidivism. This is a crisis point. Rather than facilitating rehabilitation, the system’s failures exacerbate the very conditions that drive repeat offending, particularly among those with mental health needs. There are, however, promising practices that demonstrate the perseverance, initiative, and thoughtfulness of the many community staff we interviewed, as highlighted throughout this report. By reallocating resources to the community, CSC will be able to recommend early release to more individuals while improving their prospects for reintegration, resulting in a shift in resources that will ultimately be cost neutral for the government.
The Office has previously recommended increases to the community corrections budget numerous times, with no discernable change. Given the lack of traction to-date, as a step toward proper resourcing and service delivery, I recommend that CSC:
- Double the budget allocation to community-based residential facilities, CCCs, and community mental health services, over the next five fiscal years, to meet the changing mental health profile of parolees; appropriately compensate external partners and service providers; and, ensure that community mental health and transitional services are resourced adequately.
CSC's Response: ACCEPTED IN-PART
In terms of funding, Community-Based Residential Facilities' (CBRFs) funding rose by 17.2% in 2023-24 and 6.8% in 2024-25. CSC's allocation to community corrections represented 12.4% of CSC's 2024-25 operating budget for the year, exceeding the recommendation allocation. In addition, CBRFs may offer extra services like meals, transportation, and training. These costs are part of the facility's operating expenses and help determine the daily rate CSC pays.
CSC continues to work with partners to expand and adapt services for individuals under supervision, especially those with complex health needs and provide enhanced residential Intervention funding to help CBRFs support higherrisk or higher-need individuals.
CSC Health Services is also developing post-release care plans to improve access to provincial healthcare and launching a discharge planning pilot project using a team-based approach to support inmates with complex health needs. The results will guide future policy, assessments, and training.
Next Steps: Launch of demonstration project on enhanced health discharge planning at targeted sites.
Timeline: Summer 2026
-
Implement changes to Discharge Planning and Community Mental Health by the end of fiscal 2025-2026, including the following enhancements:
- Update and streamline national policies and tools, including clear service standards and reporting requirements;
- Implement a mental health needs assessment that enables reintegration planning;
- Improve training, education, policies, and procedures around information sharing;
- Ensure compliance with policies around releasing individuals with government identification (preferably birth certificates); and,
- Remove barriers to accessing government funded health and mental health care on release by focusing on improving collaboration with provincial and territorial health authorities as well as community partners.
CSC's Response: ACCEPTED
CSC views discharge planning as a vital part of helping individuals transition from custody to the community, ensuring continuity of care. CSC has an established discharge planning process and is committed to improving it.
Discharge planning is a key responsibility of CSC to support smooth reintegration. Once individuals are in the community, provincial governments take over responsibility for health care. CSC currently provides clinical discharge planning and targeted health services to support individuals with serious health needs during their transition.
The goal of CSC's community health services is to ensure ongoing care from institutions to the community. These services include clinical discharge planning; health care for individuals living in the community, including those in Community Correctional Centres (CCCs), Community-Based Residential Facilities (CBRFs), and private accommodations.
CSC is strengthening its approach to community health services to ensure consistent, equitable, and effective support for individuals transitioning from custody to the community.
To promote service consistency, CSC is developing National Standards for Community Health Services, including discharge planning. These standards will define a baseline of services aligned with CSC policies, evidence-informed practices, and health equity principles to support inmate wellness.
To further improve continuity of care, CSC will launch a demonstration project focused on enhanced discharge planning for individuals with complex health needs. This project will use an interdisciplinary team and dedicated resources. The findings will guide future policy updates, assessment improvements, and staff training.
CSC also remains committed to helping individuals obtain government identification during their sentence, in line with its 2019 policy update. This ensures smoother access to services upon release.
As part of the Health Services Partnership Plan, CSC will continue working with partners-including provinces and territories-to expand post-release services and address barriers to accessing provincial health care.
Next Steps:
- Launch of Health Services demonstration project on enhanced discharge planning at targeted sites.
Timeline: Summer 2026
- CSC will continue to refine the Partnership Engagement plan to enhance engagement with community health services.
Timeline: Ongoing
Appendix B: Additional Information on Clinical Discharges
Table 1. Overview of Federal Releases that met the Threshold for Mental Health Discharge
| 2022-2023 | 2023-2024 | |||
|---|---|---|---|---|
| # | % | # | % | |
| Total Federal Releases* | 6,426 | 6,625 | ||
| Number of Releases Where the Criteria for Clinical Discharge Was Met** | 377 | 5.9 | 384 | 5.8 |
| No Discharge Plan | 69 | 18.3 | 52 | 13.5 |
| No Health Card on Release | 155 | 41.1 | 100 | 26 |
| Health Card Status ‘Unknown’ or ‘Requested but not Received’ | 69 | 18.3 | 75 | 19.5 |
| No Medication on Release | 19 | 5 | 20 | 5.2 |
| Unknown Medication on Release | 78 | 20.7 | 54 | 14.1 |
| Number of Individuals who Met Criteria for Clinical Discharge | 328 | 330 | ||
| Demographics | ||||
| Male | 266 | 81.1 | 268 | 81.2 |
| Female | 62 | 18.9 | 62 | 18.8 |
| Indigenous | 151 | 46 | 146 | 44.2 |
| White | 143 | 43.6 | 144 | 43.6 |
| Black | 22 | 6.7 | 19 | 5.8 |
| Individuals by Region | ||||
| Atlantic | 35 | 10.7 | 34 | 10.3 |
| Quebec | 68 | 20.7 | 73 | 22.1 |
| Ontario | 105 | 32 | 109 | 33 |
| Prairies | 97 | 29.6 | 99 | 30 |
| Pacific | 23 | 7 | 15 | 4.6 |
Source. *Data Retrieved from CRS-M on October 25, 2024. All remaining data in the table were received on October 24, 2024, through an official documentation request to CSC.
** This section represents releases, not individuals. One individual may have more than one release in a fiscal year.
An Update on Therapeutic Ranges and Intermediate Mental Health Care
According to the Correctional Service Canada’s (CSC) Mental Health Guidelines (2023), the purpose of Intermediate Mental Health Care (IMHC) is to provide mental health support and treatment for incarcerated individuals who have needs that are higher than what can be addressed in primary care, but who do not meet the criteria for, or who do not consent to, care at a Regional Treatment Centre (RTC). Although commonly offered in a designated unit, IMHC is a level of service that can be delivered anywhere in the institution. IMHC services were first launched at women’s institutions in 2001 with the establishment of the Structured Living Environments (SLE). In 2016, they were introduced at a men’s maximum-security facility and have since been rolled out at multiple maximum- and medium-security institutions across all regions.
In 2019-2020, the OCI conducted a national systemic investigation into IMHCs at standalone maximum-security institutions, which are more commonly referred to as Therapeutic Ranges (TR). The investigation identified multiple gaps, including:
- Underutilization of Therapeutic Ranges and placement of individuals not requiring IMHC on Therapeutic Ranges, often as a population management measure.
- Deficiencies in the therapeutic look-and-feel of Therapeutic Ranges, which often appeared no different than traditional segregation units.
- Staffing complements that did not reflect institutional needs, a strong security presence, and a high turnover of senior mental health staff.
Further to these findings, the Office recommended that CSC conduct an “external review of its Therapeutic Range resourcing model and to ensure that bed capacity and staffing reflects the actual needs of Mental Health Services.” The Office also recommended that CSC consider several improvements, including the therapeutic look and feel, dynamic security, and dedicating an adequate complement of correctional and mental health staff.
CSC’s IMHC Review
From September 2020 to December 2022, CSC conducted an internal review of IMHC across all institutions (except RTCs) and shared the final report and findings with our Office in January 2023.101 This review was carried out by a working group led by CSC’s National Senior Psychiatrist and in consultation with twelve external experts, with the explicit intention of fulfilling its commitment against Recommendation 13 of the 2019-2020 Annual Report of the OCI. Although not external, the review did fulfill part of our previous recommendation. The working group not only looked at IMHC in the standalone maximum-security units, but also included IMHC in men’s medium- security institutions and women’s institutions. The findings and 38 recommendations mirrored and went beyond what this Office reported in 2019-20. Some highlights of the recommendations put forward to CSC by the working group include:
- Promote national consistency in the application of clinical admission/discharge criteria.
- Review the existing infrastructure and physical environment of IMHC units to support a therapeutic environment and facilitate treatment interventions, recovery, improved functioning, and quality of life.
- Implement evidence-based individual and group mental health assessment and treatment services that are available at all IMHC sites covering the most prevalent mental health needs.
- Assign dedicated correctional officers to men’s IMHC units in a Therapeutic Officer role to facilitate interactions and achieve treatment and programming goals.
Current Investigation
It’s been five years since the Office published its findings and recommendations on Therapeutic Ranges. Given our thematic focus on mental health care in corrections for this year’s annual report, it would be remiss of the Office not to conduct a follow-up review of the Therapeutic Ranges and to investigate IMHC more broadly. Accordingly, we reviewed progress on past recommendations for Therapeutic Ranges – both from the OCI and CSC’s working group – and conducted a cursory review of IMHC delivery at men’s medium-security institutions, given that we have not previously assessed the IMHC rollout in medium security. This was done through documentation requests, questionnaires to all six maximum sites,102 correspondence and site visits, as well as interviews with 15 staff members and eight incarcerated individuals. The purpose of the investigation was to provide a snapshot of IMHC in men’s maximum and medium institutions and report on the status and progress of IMHC, including gaps and challenges. Based on our investigation, our findings are as follows:
- Overall progress in Therapeutic Ranges remains stagnant.
- Lack of a standardized approach results in inconsistent care and competing demands.
- Inadequate infrastructure hinders a therapeutic environment.
- Dynamic security and trained staff are lacking.
- Discontinuity of care leads to a revolving door.
Our past observations of Therapeutic Ranges and intermediate care units were that they are not providing the level and quality of mental health care to address the needs of their patients. In fact, we have previously stated that those units are only therapeutic in name. CSC’s own internal review supported our observations. With the implementation of the new 2019 Structured Intervention Units (SIUs) provisions, resources have been redirected to SIUs and CSC’s corporate focus has shifted away from intermediate mental health care. Our initial assessment that those therapeutic units operate only in name is as true today as it was five years ago.
Findings
Profile of IMHC at Standalone Maximum-Security Institutions (Therapeutic Ranges)
As can be seen in Table 1, out of the six standalone maximum-security institutions, four currently have a living unit dedicated to IMHC (i.e., Therapeutic Range), including 92 funded beds, with a budgeted complement of approximately 27 staff and an annual allocation of $1.8 million.103 As of March 2025, there were no Therapeutic Ranges in the Quebec region. According to the IMHC Review report, IMHC was available at Port Cartier Institution in Quebec during the review period but that no longer seems to be the case, based on our correspondence with the site. At Donnacona Institution, there were plans to convert part of the 96-bed unit into a Therapeutic Range (the unit has not been in use for approximately five years), but plans were delayed due to unresolved issues with infrastructure, as well as staffing and security concerns. With a planned opening of its Therapeutic Range on April 15, 2025, staff at Donnacona shared that interim measures are in place to manage individuals with mental health needs. These measures include appointments with psychiatrists as needed and regular follow-ups; ongoing monitoring and care by a team of mental health professionals; and, transfers to the Regional Mental Health Centre (RMHC) in cases of serious need or acute distress. While these stopgap measures are necessary, having an entire region without IMHC at the maximum-security level for an extended period of time has inevitably put pressures on primary-level care and has resulted in inconsistent and inadequate mental health support for individuals.
Table 1. Resourcing for IMHC at Men’s Standalone Maximum-Security Institutions
| Institution | Region | Designated TR Unit | Budgeted Staff | Actual Staff* | Funded Beds | Unfunded Beds* | IMHC Allocation |
|---|---|---|---|---|---|---|---|
| Atlantic | Atlantic | Yes | 7 | 0 | 30 | 0 | $560,983 |
| Millhaven | Ontario | Yes | 5 | 5 | 20 | 3 | $548,234 |
| Edmonton | Prairie | Yes | 5 | 2 | 18 | 6 | $244,054 |
| Kent | Pacific | Yes | 5 | n/a | 24 | n/a | $437,470 |
| Port Cartier | Quebec | No | -- | -- | -- | -- | -- |
| Donnacona | Quebec | No | 5 | -- | -- | -- | $25,469 |
| Total | 4 out of 6 | 27 | 7 | 92 | 9 | $1,816,210 |
Source: Data received from CSC on April 23, 2025.
* Data for actual staff and unfunded beds are based on responses received via institutional questionnaires conducted in fall 2024.
Profile of IMHC at Men’s Medium-Security Institutions
According to documentation provided by CSC, IMHC is currently provided at seven men’s medium-security institutions104 (see Table 2), and includes 136 funded beds, with a budgeted complement of approximately 39 staff and an annual allocation of over $3 million.105 The provision of services and a designated unit does not, however, appear to be consistent nor sustained. For example, some sites that previously had IMHC services reported that these no longer exist due to a lack of resources and staffing. Capacity and bed usage at the mediums varied by site, with some being manageable and others struggling with waitlists, particularly in regions where IMHC was only available at one institution.
Table 2. Resourcing for IMHC at Men’s Medium-Security Institutions
| Institution | Region | Designated IMHC Unit | Budgeted Staff | Funded Beds | IMHC Allocation |
|---|---|---|---|---|---|
| Dorchester | Atlantic | Yes | 5 | 20 | $508,266 |
| Federal Training Centre | Quebec | Yes | 5 | 20 | $611,114 |
| Archambault* | Quebec | No | 5 | N/A | $332,791 |
| Bath | Ontario | Yes | 7 | 38 | $589,304 |
| Warkworth | Ontario | Yes | 5 | 20 | $482,193 |
| Stony Mountain | Prairies | Yes | 7 | 22 | $264,842 |
| Matsqui | Pacific | Yes | 5 | 16 | $428,297 |
| Total | 6 out of 7 | 39 | 136 | $3,216,807 |
Source: Data received from CSC on April 23, 2025.
* Archambault does not have a designated IMHC unit or a designated number of beds as care is provided on an ambulatory basis.
Overall Progress in Therapeutic Ranges Remains Stagnant
What we found in the Therapeutic Ranges was disheartening and showed clear evidence of inertia, with little indication of meaningful change in the last five years. When asked about overall progress and what efforts had been taken to improve the Therapeutic Ranges, one site noted nothing has changed since the Office reported on the units in 2019-2020. Another site listed several efforts they had attempted to improve the unit (e.g., programming in unit, garden programs, pet therapy) but voiced frustrations around barriers, as most requests had been denied by management due to ‘operational resources.’
Compared to the Therapeutic Ranges in maximum, it appears some progress has been made in the delivery of IMHC at medium-security institutions. Staff noted the importance of providing one-on-one mental health support on these units. Current treatment approaches include individualized treatment plans, more frequent and regular interactions with mental health staff, more direct supervision, medication management, as well as individual and group-based interventions. Most medium IMHC sites also offer therapeutic activities outside of interventions (e.g., access to sensory rooms, garden space, walking and book clubs). Staff did note, however, that implementation of these improvements was not without its challenges, with multiple requests being denied or taking exceptionally long for approval, due to purported ‘security and operational resource’ issues. As one IMHC resident stated, “[mental health] staff are doing their best and they’re racking their brains, but [management] are going to keep putting obstacles in their way.” Despite some signs of progress in medium security, overall, challenges and significant gaps remain.
Lack of Standardized Approach Results in Inconsistent Care and Competing Demands
A fundamental issue with IMHC overall and one that was raised at both the maximum and medium security sites, is the lack of standardized care and guidelines. This was flagged as a gap in the IMHC Review report where they noted that, although men’s institutions have consistent staff requirements and the same admission/discharge criteria, “they have no common requirements for infrastructure or mental health programs.” Because of this, the report recommended CSC initiate the following:
“Institute a National Advisory Group for IMHC to oversee the Service, and promote national consistency, quality of care and quality improvement, including through setting national standards for IMHC [...] Create a Community of Practice for staff working with the IMHC population.”
Review of Intermediate Mental Health Care Services in Correctional Service Canada Mainstream Institutions and Associated Recommendations: Overview, Purpose, Principles and Process (CSC Report, January 2023)
Despite these recommendations being issued in 2023, we heard from the sites that standard guidance is “non-existent” and there is little understanding of the role and purpose of the IMHC, particularly from management. Staff noted this lack of a standard vision has resulted in varying approaches between sites, with no centralized mechanism for sharing information or resources. Staff also shared that when the IMHC model was first rolled out, they were told to establish entirely new units and to devise new approaches to mental health care, while receiving minimal guidance from NHQ, no evidence-based recommendations, tools, or support. Consequently, incarcerated individuals needing intermediate care are likely getting different, inconsistent, and/or inadequate supports and interventions across institutions and regions.
In addition to inconsistent care, without a clear vision and standardized approach, IMHC is getting lost in the evolving world of mental health services and competing demands in corrections. For example, staff at the standalone maximums reported multiple challenges in addressing the needs of IMHC patients as staff are often preoccupied with demands outside of Therapeutic Ranges, such as the Structured Intervention Units (SIUs). As this Office has reported, SIUs have been notorious for diverting mental health resources at maximum security institutions, as explained by the following interviewee, “There is no standard. The system had a great run right up until the SIUs opened, and then suddenly it [IMHC] was put on the back burner. We still get the same guys, but now we have no resources, nothing to deal with them, and there are no guidelines for anything. Honestly, the only thing in the guidelines is the complement of staff. [And] we don’t have it.”
Inappropriate Use of IMHC Beds
In the same vein of insufficient standards and competing demands, concerns were also raised regarding competing views on admission criteria and decision-making authorities. Some sites reported continued disagreements with operations staff who insist on using unfunded beds in the Therapeutic Range to “relieve operational pressures.” One staff member shared that even though IMHC placement decisions are “supposed to be made strategically,” operational staff had been using the range as, “a dumping ground.” Another staff member put it as follows: “It’s the same as the SIU now, they dump guys here who have interpersonal conflicts elsewhere, or who are just afraid to be in prison. That’s not mental health.”
While less common in the medium facilities, this issue did come up. Staff stated this practice can have a significant impact on the IMHC residents, interfering with their mental health care and the stability of the unit. This concern links directly to one of the IMHC Review recommendations that “clinical admission and discharge to and from these Units should be a health care decision based on clinical criteria”; a recommendation the OCI fully supports.
Inadequate Infrastructure Hinders a Therapeutic Environment
The issue of therapeutic environment has come up multiple times in our previous reporting and in the CSC IMHC Review report. For the most part, Therapeutic Ranges at maximums remain very similar in appearance to the old segregation units, despite some of the efforts by well-meaning staff. When asked what steps had been taken to improve the environment, one site shared that they had painted areas of the Therapeutic Range to provide a more therapeutic look and feel, only to have the area repainted as they had not obtained the proper approvals. Another site could only offer the following: “The Therapeutic Range does not receive regular access to the [gym or large yard]. Our patients often refuse to attend small yard due to its exposure to other units through their windows and the [TR] staff have received reports of verbal abuse between offenders. […] Our range does not have accessible cells, regular use of an elevator or an accessible shower, which limits our ability to admit offenders with specific mobility challenges.”
At the mediums, individuals we spoke with noted challenges with the physical infrastructure, citing insufficient space for both incarcerated individuals and staff, and a limited therapeutic environment. Some sites also raised concerns regarding the visibility of the unit, noting that the lack of privacy can increase the stigma and victimization experienced by IMHC residents. When mental health care units are indistinguishable in appearance and feel from other areas of the prison, it is unreasonable to expect much improvement in patients or a shift in culture among staff. As it stands, the physical environment of IMHC units is neither conducive to, nor consistent with, proper mental health care.
Dynamic Security and Trained Staff are Lacking
While all sites seemed to agree with the need to employ specially trained operations staff (e.g., Therapeutic Unit Officers)106 who have specific interests in engaging with patients, dynamic security, and collaborating with Mental Health Services staff, this was not always the case in practice. For example, the Therapeutic Unit Officer position, one that was recommended by the OCI and the IMHC Review, has, for the most part, been poorly implemented in the max units. Here is how one staff member described the problem, “We used to have a Therapeutic Officer dedicated to the [TR] unit, but no such position exists currently to assist with programs. Additionally, this has created tension between departments as operations has been in conflict over this position and mental health staff are caught in the middle.” Another staff member stated, “There is a [Therapeutic Range] officer on each day shift, but they do not have specific training related to mental illness or mental health service delivery. They also rotate through as shift workers, diminishing their ability to gain rapport with our patients and gain an appreciation for the functioning of the range.”
Staff acknowledged there are some operational staff who voluntarily work on the IMHC units and who genuinely have an interest in working with this type of population; however, others are not suited to working with people with mental health needs. Proper training and implementation of the Therapeutic Unit Officer role could help to mitigate many of these issues.
Beyond the officer position, challenges with staffing vacancies were also reported, particularly with psychology staff. Recruitment and retention continue to be issues with negative consequences, such as reduced opportunities for psychological support and a limited capacity to conduct diagnostic assessments. The importance of hiring, training, and maintaining consistent, experienced, and specialized staff for the stability of patients was frequently underlined by staff and is a concern shared by this Office. With vacancies, the burden of work inevitably falls to others who are being asked to do more with less. Without adequate support, staff burnout and negative impacts on the IMHC population are unavoidable.
Discontinuity of Care Leads to a Revolving Door
Both staff and incarcerated individuals raised concerns about the continuity of mental health care; specifically, the transition from IMHC into general population and release to the community. Among other concerns, they highlighted a notable gap in the availability of, and access to, mental health supports once an individual leaves IMHC. In some cases, individuals were discharged from IMHC only to struggle in the general population and return to the unit multiple times. Similarly, there were cases where individuals were released and then quickly revoked while under community supervision. One site even disclosed that they have implemented a practice of keeping an individual’s bed available for a period of time after they have been released in the community, with the expectation that they may soon return. Understandably, we heard from staff that requiring IMHC support multiple times throughout one’s mental health journey is not necessarily negative. However, if individuals are coming back into IMHC through a revolving door because they cannot access adequate services, then the system has failed them.
Conclusion
It has been nearly ten years since the introduction of IMHC services at men’s institutions, five years since the OCI published its investigation into Therapeutic Ranges, and more than two years since CSC’s review of IMHC services. During that time, millions of dollars have been invested into this service. Through this investigation we sought a response from the Service on evidence of progress made against the recommendations that have been put forward to them on IMHC. Consistent with what we observed during our site visits and interviews, CSC’s responses were vague and lacking evidence of substantial, concrete progress.
In the final paragraphs of its 2023 IMHC report, the working group stated that “Further review of the recommendations will be important in the consideration of effective implementation strategies to support continuous improvement of CSC’s intermediate mental health care services.” While we largely agree with the findings of the report, this statement falls disappointingly short of what is required at this stage. No further reviews are needed. Interviews with CSC staff and external stakeholders strongly suggest a growing prevalence of mental heath needs and co-morbid substance use disorders among federally sentenced individuals. The need for effective mental health interventions will only continue to grow. Action, by way of implementation of the recommendations put forward by both this Office and CSC’s own working group, is the necessary next step.
I recommend that the Correctional Service of Canada:
- Immediately respond to the recommendation and issues previously raised by the OCI regarding Therapeutic Ranges and the provision of intermediate mental health care.
CSC's Response: ACCEPTED
CSC acknowledges the previously received recommendations from the Office of the Correctional Investigator (OCI) and will use this to inform enhancements to CSC's continuum of care.
CSC, in consultation with external experts and led by its National Senior Psychiatrist, conducted a thorough review of Intermediate Mental Health Care (IMHC), including Therapeutic Ranges (IMHC in maximum security institutions) in response to the recommendations made by the OCI. The primary purpose of the IMHC review was quality improvement, particularly with respect to improving mental health outcomes, functioning and quality of life for inmates with mental illness. The recommendations highlighted several priority areas, including standardization of processes, staffing composition and roles/responsibilities; discharge planning and transitions of care; and enhanced collaborative approaches with intersectoral partners.
Guided by the report, CSC developed four key objectives for 2025-26:
- Deliver individual and group treatment at all IMHC sites
- Provide IMHC-level care in ambulatory settings across all institutions
- Provide standardized diagnostic assessments at all IMHC sites
- Ensure Activities of Daily Living (ADLs) are offered at all IMHC sites
CSC will be implementing enhancements to the IMHC model to standardize service provision in response to recommendations stemming from this review and the OCI's recommendations.
Next Steps: CSC will review Intermediate Mental Health Care services to support service standardization.
Timeline: Fiscal year 2025-26
-
Immediately respond to and action each of the 38 recommendations outlined in the IMHC Working Group report titled, “Review of Intermediate Mental Health Care Services in Correctional Service Canada Mainstream Institutions and Associated Recommendations” (January 11, 2023). Specifically, I recommend that CSC:
- Develop and publicly report on a plan addressing and responding to each of the 38 recommendations individually with concrete actions and timelines by the end of fiscal year 2025-2026.
- Ensure complete implementation of each of the 38 recommendations by 2026-2027.
CSC's Response: REJECTED
CSC is currently implementing enhancements to the IMHC model based on the recommendations provided by the OCI and the associated "Review of Intermediate Mental Health Care Services in Correctional Service Canada Mainstream Institutions and Associated Recommendations” (January 11, 2023) completed by CSC. The initial priority areas of focus will be the standardization of assessment and interventions across IMHC units, the provision of IMHC on both a unit-based and ambulatory basis to better meet the health needs of the inmate population, and enhanced data and monitoring. Additional recommendations from the report will be assessed for implementation moving forward.
Additionally, CSC will begin publicly releasing a CSC health system overview and quality score card in Summer 2025. The document will provide an overview of the health needs of inmates and the performance of CSC's health system from an inmate and quality improvement perspective. The CSC Health System Overview and Quality Score Card will support ongoing sharing of data to understand population health needs and health outcomes and to support a culture of quality improvement within CSC. This evergreen report will be published online and shared with key stakeholders annually.
Next Steps: CSC will review Intermediate Mental Health Care services to support service standardization.
Timeline: Fiscal 2025-26
Assessing and Addressing Trauma in Federally Sentenced Women
Although difficult to quantify, it is widely acknowledged that most women107 who come into contact with the criminal justice system have histories of trauma and victimization. Their life experiences are deeply intertwined with their involvement in the justice system and cannot be easily separated from the circumstances that led to their incarceration. For this investigation, the Office of the Correctional Investigator (OCI) collaborated with the Office of the Federal Ombudsperson for Victims of Crime (OFOVC). This unique partnership brought an added layer of rigour and compassion to the investigation. It also provided a safe and supportive context for incarcerated women to share how they have navigated their federal sentence while carrying the burden of past trauma and victimization. The collaboration enabled a truly trauma-informed approach to the work.
I extend my sincere appreciation to Dr. Benjamin Roebuck, Canada’s Federal Ombudsperson for Victims of Crime, and his team for their insight and support. Their professionalism and subject matter expertise greatly enriched this investigation and offered us a renewed understanding of the complex challenges facing federally incarcerated women.
Trauma is the lasting emotional response that often results from living through a distressing or disturbing event. These experiences can significantly undermine a person’s sense of safety, identity, and ability to regulate emotion. Long after the event, individuals may continue to experience shame, helplessness, fear, and emotional dysregulation.108
Research, including CSC’s own data, has shown that federally sentenced women are disproportionately affected by trauma, including high rates of interpersonal trauma, victimization, Post-Traumatic Stress Disorder (PTSD), and exposure to violence.109 For Indigenous women, the impacts of trauma are often intergenerational, historical, and collective. Although trauma is not formally recognized as a criminogenic need by CSC’s risk assessment tools, there is a strong and well-documented link between trauma and women’s criminalization.110 As a result, CSC has a unique responsibility to understand and address the impact of trauma. This investigation explores how trauma is assessed and treated in the federal correctional system, and whether current approaches are gender- responsive, culturally relevant, and trauma-informed.
Current Investigation
In conducting this investigation, the following methods were utilized:
-
Site visits were conducted at the following institutions:
- Fraser Valley Institution (FVI)
- Edmonton Institution for Women (EIFW)
- Joliette Institution for Women (JIFW)
- Regional Psychiatric Centre (RPC) – Assiniboine Unit
- Qualitative interviews were conducted with a total of 36 incarcerated women. Questions focused on how their histories of trauma are acknowledged and handled in the carceral setting, interactions with staff, exposure to triggering events, and access to mental health services and/or relevant programming.
- Qualitative interviews were also conducted with 34 institutional staff and management. These questions focused on available training and tools related to trauma and trauma-informed practices, staffing and resources, and operational challenges.
- Review of relevant literature related to trauma and incarcerated women.
- Review and assessment of CSC research, programs, training materials, services, and interventions.
Trauma-Informed Approach vs. Trauma-Specific Treatment
While often used interchangeably, these terms refer to different, but related, concepts:
- A trauma-informed approach requires an understanding of the effect of trauma on individuals and its link to mental and physical health problems, substance abuse, behavioural challenges, and brain development. It involves integrating this knowledge into policies and practises to minimize damage or re-traumatization.
- Trauma-specific treatment refers to the provision of therapeutic approaches that are specifically designed to address trauma and related symptoms, with an aim of facilitating healing and recovery.
Findings
The Prison Environment as a Source or Trigger of Trauma
“I think it’s honestly adding more trauma to my life. I came here with a lot of trauma and I feel like I’m going to leave with more trauma than I had in the first place (…) I isolate a lot because I don’t have anybody to connect with (…) I just sit there. I have depression, anxiety, PTSD, and a panic disorder, and I start to get more depressed. I’m noticing that I’m withdrawing from the activities that I used to enjoy.”
Incarcerated interviewee
Incarceration itself can be a traumatic experience. Many women told my Office that the prison environment—hostile, often violent, and marked by a lack of autonomy—has worsened their mental health, retriggered past traumas, or resulted in new traumatic experiences. Some described feeling constantly on edge or emotionally fatigued. Routine institutional practices, including strip searches, cell searches, institutional counts, lockdowns, and recounting one’s story to new staff were consistently identified as triggering. Women said these practices often lead to trauma-related behaviours such as aggression, withdrawal, and impulsivity.111 These behaviours are rarely understood as trauma responses and are often met with security-based responses like the use of force, loss of privileges, or, in some instances, placement in the Structured Intervention Unit (SIU).
At the same time, many women expressed a strong desire to work on their trauma while incarcerated. They acknowledged that, despite the institutional barriers, this may be the only period of their lives where they are able to reflect, pause, and begin the healing process. As one woman explained, “It’s the best place. I committed a homicide because of my grief and trauma (…) This is what we need to work on. This is the only place. This is when we have time to do it. As soon as we get out, we don’t have time to do it. When are we going to do it? When you’re in the halfway house and have to work?”
CSC programs like Dialectical Behaviour Therapy (DBT) focus on helping women cope with emotional dysregulation and impulsivity. These approaches are helpful, but they are not the same as trauma-specific therapy. Many women told us that programs focused on coping skills are only “scratching the surface.” They want the opportunity to explore and address the underlying trauma.
In the absence of formal trauma counselling, many women said they are doing their best to self-regulate and cope through exercise, spirituality, art, and peer support. While commendable, these strategies often require support from trained professionals to be effective and safe. One woman describes her willingness and reluctance to seek help in these words, “There is no safe space to share here. If that was existent, I would have done it and I would be doing it. I’m willing to do anything and everything.”
Although there are associated challenges, there is academic evidence to suggest that trauma processing therapies, and individual trauma-focused interventions can be effective and delivered successfully in prison.112 However, existing options, such as the Regional Psychiatric Centre (Prairies) or Healing Lodges, are not currently structured or resourced to meet the needs of women with complex trauma.
Absence of Assessment and Screening for Trauma
Effective screening and assessment are critical to ensuring appropriate treatment and intervention. In the federal correctional system, the Computerized Mental Health Intake Screening System (CoMHISS) is the primary standardized tool used to identify individuals requiring mental health services. It consists of five distinct screening tools that assess various psychological symptoms and risks. However, CoMHISS does not include specific screening for trauma exposure, nor is it tailored to gender or cultural contexts.
One widely recognized tool for trauma screening is the Adverse Childhood Experiences (ACEs) questionnaire. ACEs such as abuse, neglect, and household dysfunction are strongly associated with increased risk of chronic health issues, mental illness, substance use, and even premature death.113 Although CSC does not routinely screen for ACEs, a 2023 CSC study explored their prevalence and impact on institutional and community outcomes. The study found that ACEs are common within the federal offender population, particularly among women and Indigenous women. ACEs were linked to negative correctional outcomes, and the study recommended using this knowledge to inform more responsive case management strategies and interventions.114 Despite these findings, CSC has not implemented a trauma or ACEs-specific screening tool. As a result, the Service remains ill-equipped to adequately assess trauma in order to offer comprehensive trauma-informed or trauma-specific interventions.
In the absence of formal screening, both incarcerated women and CSC staff told my Office that traumatic life experiences are typically brought up during intake or programming. However, these discussions are primarily focused on the link to criminal behaviour and used for assessing risk and need and not for therapeutic purposes. Consequently, many women reported reluctance to disclose trauma due to fears that the information could appear in official reports or be used against them. They also shared that discussing deeply painful experiences often leaves them feeling ashamed, overwhelmed, and unsupported. One woman recounted how disempowering it felt to read this excerpt from her Correctional Plan, after disclosing her trauma: “File and interview information indicated that she was a behavioural problem as a child. She reported being sexually active since age eight. She has been able to develop communication skills as a means of personal survival that contributed to her well- established ability to defraud in adulthood.” This kind of risk-based assessment and reporting is not trauma-informed. It can cause significant harm and undermines rehabilitation efforts.
Inadequate Training Related to Trauma and Trauma-Informed Approaches
Building a trauma-informed organization requires more than awareness. It demands a deep understanding of how individuals perceive, adapt to, and respond to trauma, as well as a commitment to revising practices that may inadvertently trigger past experiences or feelings of helplessness.115 In practical terms, CSC staff must not only recognize the widespread impact of trauma but also understand how it can manifest behaviourally and emotionally within a correctional environment. This commitment must be embedded across all levels of operations.
However, many CSC staff interviewed by my Office reported that the current training provided—primarily the National Training Standards and the Trauma-Informed Approach Kit available on CSC’s Hub—is viewed as basic, repetitive, and inadequate for preparing staff to manage the complexities of trauma or work effectively with individuals with complex needs. In describing this gap, a parole officer told my staff, “I often take advantage and seek out supplementary training; there is some in the women-centred training, but it is rudimentary.”
Although most staff could articulate a general understanding of what a trauma-informed approach entails, many lacked a deeper comprehension of how trauma histories can influence behaviour in custody, or how routine correctional practices might be triggering. While some practices, such as strip searches, were easily recognized as potentially harmful, others (e.g., loud noises, aggressive communication, physical contact, and the use of flashlights during nighttime counts) were not identified as triggers and were seen as standard, unavoidable aspects of the correctional setting.
Most concerningly, several staff acknowledged that while being trauma informed is important in theory, in practice, any behavioural incident still prompts a default security response, often at the expense of a supportive or therapeutic one. A CSC staff, when asked about trauma-informed approaches, described it best when they said, “That’s all good, until it turns into a security incident.”
Insufficient Psychology Resources
My Office has repeatedly raised concerns about the planning and delivery of mental health services within federal institutions. Unsurprisingly, the most frequently cited reason for CSC’s inability to provide trauma-specific treatment is a lack of resources. Given the high-needs population and limited availability of psychological services, the majority of resources are directed toward those with the most acute or urgent needs. As a result, individual counselling for non-emergency issues is difficult to access, often with significant wait times.
Both CSC staff and incarcerated women told my Office that, in the absence of consistent and accessible psychological treatment, pharmaceutical interventions are commonly used to manage symptoms and behaviours associated with trauma. One woman described a typical scenario as follows: “You get pharmaceuticals here until you’re blue in the face (…) That’s not a long-term solution. Let’s get some long-term solutions going. Otherwise, you’ve got people who are traumatized and addicted.” Another woman noted, “It’s the cheap counsellors. A medicated inmate is easier to manage.”
In response to this gap, psychologists at some women’s institutions have taken the initiative to offer adapted group counselling sessions that focus on trauma. While these efforts reflect best practice, they are not formally supported or funded and rely entirely on individual initiative.
As noted earlier, other staff such as Elders, Behavioural Interventionists, Parole Officers, and Primary Workers are often left to support women working through trauma. Despite their genuine desire to help, they often lack the training, tools, and clinical expertise to do so safely and effectively. This not only increases the risk of harm to the women in custody but also places staff at high risk of experiencing vicarious trauma.
It is essential that trauma-specific interventions be delivered by properly trained and qualified professionals. The recent change in title from Behavioural Counsellor to Behavioural Interventionist reflects a recognition that these staff are not licensed mental health professionals and should not be providing counselling. Nevertheless, virtually every Behavioural Interventionist interviewed by my Office reported being relied upon for trauma-related support and counselling, particularly for women participating in Dialectical Behaviour Therapy (DBT), a program in which traumatic experiences are frequently explored.
Need for Culturally Specific Trauma Interventions
Indigenous women face unique and compounded challenges related to trauma, stemming from the intersection of historical and intergenerational trauma, systemic oppression, and gender-based violence. Their needs are complex and deeply rooted in the lived experiences of colonization, displacement, and marginalization. Effective healing and trauma treatment for Indigenous women requires culturally grounded approaches that honour traditional practices and reflect Indigenous worldviews. A CSC staff summarized the issue as follows: “What some people don’t understand is that you can’t separate mental health from race and culture—the two go hand in hand. If you try to see it through one type of lens, you’re not going to get it. And another thing that’s often forgotten is the generational trauma, in addition to what the ladies go through in their lives (…) We try and catch that at admission with the mental health form, but it goes far beyond that.”
Disappointingly, interviews conducted by my Office revealed a widespread lack of understanding among CSC staff about Indigenous history, culture, and the trauma Indigenous women carry and how these experiences can manifest in a correctional setting. In addition, there was little evidence of sustained efforts to promote, support, or accommodate the roles of Elders and Indigenous staff in providing culturally relevant support. Barriers to holding regular traditional ceremonies and cultural activities further undermine efforts to foster a healing, trauma-informed, and culturally responsive environment.
Conclusion
There is a critical and unmet need for incarcerated women to process and heal from their trauma. Without this foundational work, their ability to meaningfully engage in other correctional programming is severely compromised. Unaddressed trauma can worsen physical and mental health outcomes and significantly hinder successful reintegration. As one CSC psychologist aptly described, “It’s like they’re trying to rearrange the furniture in their head, while the house is burning down.”
CSC has both the opportunity and the responsibility to implement trauma screening and assessment practices that inform more comprehensive, individualized, and effective correctional planning within an environment that is truly trauma-informed.
-
I recommend that CSC works closely with an external, expert mental health organization to develop an evidence-based, comprehensive strategy for trauma-informed services and trauma-specific treatment for federally sentenced women. This strategy should include:
- Standardized screening for trauma, victimization, and Adverse Childhood Experiences (ACEs);
- Implementation of trauma-informed practices across CSC policies and procedures, supported by specialized staff training;
- Access to gender- and culturally-responsive trauma-specific therapy and counselling; and,
- Safe, supportive environments for women to begin the healing process.
The new strategy should be fully implemented by June 2026. The new model should then be evaluated by CSC, and a similar approach extended to male institutions nationwide.
CSC's Response: ACCEPTED IN-PART
CSC acknowledges the impact of trauma in the incarcerated population and has implemented an integrated primary care model aligned with the Patient's Medical Home Model from the College of Family Physicians of Canada. This model is a comprehensive· person-centered care approach that integrates team-based, trauma-informed care within a quality improvement framework. This model emphasizes collaboration, inmate engagement and a clear, structured approach to providing integrated care for physical and mental health that meets the unique needs of each incarcerated individual.
Trauma-informed care is grounded in understanding and being responsive to the impact of trauma. Given the prevalence of past trauma and the impact to inmate mental health and criminogenic risk, a trauma-informed approach to address an individual's mental health needs can facilitate better therapeutic rapport as well as better treatment outcomes. Need for trauma counselling is assessed on a case-by-case basis and when indicated would be provided by trained mental health professionals. Additionally, Dialectical Behaviour Therapy (DBT) and Integrated Modular Therapy (IMT) are comprehensive therapeutic interventions that involves learning and developing strategies to help manage emotional regulation and can be an effective treatment for inmates with trauma histories.
CSC has provided health staff training on trauma-informed approaches that includes both theory and application in a correctional environment. In 2022-23 we have also provided trauma-informed for offenders training to all Parole Officers.
CSC has engaged with and funded community partners who deliver traumainformed services and life skills counseling to support the mental health and wellbeing of women. CSC will continue to seek important internal and external partnerships to support the provision of trauma-informed interventions.
A greater proportion of Indigenous people in custody report histories of complex trauma. Foremost is the impact of the intergenerational trauma effects that are passed down from one generation to the next to Indigenous peoples. Efforts to ensure relevant Indigenous Social History and a holistic approach with the inclusion of Elders/Spiritual Advisors, Elder Helpers and Chaplains are considered during the provision of health services.
In 2025, CSC is introducing updated Women Centred Training which includes trauma-informed approaches. The target audience for training has been expanded to include all staff working at women's institutions and will contribute to safe and supportive environments.
Next Steps: CSC will continue to refine the Partnership Engagement plan to enhance engagement with community health services.
Timeline: Ongoing
Mental Health Needs and Services for Indigenous Peoples in Federal Corrections
“Indigenous peoples have the right to their traditional medicines and to maintain their health practices, including the conservation of their vital medicinal plants, animals and minerals. Indigenous individuals also have the right to access, without any discrimination, to all social and health services...Indigenous individuals have an equal right to the enjoyment of the highest attainable standard of physical and mental health. States shall take the necessary steps with a view to achieving progressively the full realization of this right.”
United Nations Declaration on the Rights of Indigenous Peoples (UNDRIP)
The disparities in mental health and access to quality care for Indigenous peoples in Canada has been well documented. These disparities are firmly rooted in the long legacy of colonialism, intergenerational trauma, and barriers to services for the Indigenous population generally. In 2024, Statistics Canada reported that among Indigenous peoples requiring mental health care, approximately three quarters reported that their needs were not being met.116 Furthermore, roughly one in five Indigenous peoples reported experiencing unfair treatment, racism, or discrimination from a health care professional. Many factors, such as the key social determinants of mental and physical health, including poverty, unemployment, food and housing insecurity, are experienced at higher rates and severity among Indigenous peoples and communities. The impacts of such factors on mental health are further compounded by the unique effects of intergenerational trauma (e.g., Residential School system, the Sixties Scoop, Child Welfare policies), discrimination, and social exclusion. Consequently, in many cases, these socio-historical factors materialize in individuals as higher rates of significant mental health conditions, including depressive symptoms and disorders, suicidality and self-harm, post-traumatic stress disorders, and co-occurring mental health and substance misuse disorders.
Due to the criminalization of those with mental health concerns, and the over- representation of Indigenous peoples in prison overall (who account for approximately one third of all individuals in federal custody), the prison system is now, more than ever before, filled with Indigenous individuals with complex health needs. In fact, numerous studies have specifically examined the prevalence of the mental health needs of Indigenous peoples serving federal sentences, finding that Indigenous men and women have consistently higher rates of mental health issues compared to their non- Indigenous counterparts.117 For example, studies using clinical interviews of individuals upon admission have found that 94% of Indigenous men and 97% of Indigenous women reported having had a mental health condition at least once in their life.118 For Indigenous women specifically, research has found up to 100% of Indigenous women in study samples met the criteria for a lifetime diagnosis of a mental disorder and upwards of 96% met the criteria for a current mental disorder. The most common diagnoses for Indigenous women were antisocial and borderline personality disorders, and among the most commonly diagnosed anxiety disorder was PTSD, affecting nearly one third of the women meeting the criteria for that disorder group.119 Relatedly, the high incidence of self-harming behaviours among Indigenous men and women alike, are inextricably linked to the high rates of mental health concerns among this population. Specifically, more than half of incidents of self-injury in federal corrections in recent years have involved an Indigenous person.120
Taken together, these research findings were corroborated by the perspectives and experiences shared by of the individuals with whom we spoke over the course of this investigation. Many expressed concerns regarding not only the sheer numbers of Indigenous individuals living with significant mental health needs within the prison system, but also described the various difficulties in meeting their needs. Some individuals cited a notable shift in the severity of mental health conditions in recent years, including issues such as the complexity of co-occurring mental health disorders, drug- induced mental health symptoms and disorders, including brain injuries and neurological complications from prolonged drug use, as well as multi-faceted and long-standing emotional traumas.
Current Investigation
In the context of this annual report’s focus on mental health in corrections, the Office undertook a review of the mental health needs, current approaches to services offered, as well as the gaps and barriers to addressing mental health for Indigenous prisoners. Through the course of this review, we consulted the literature and spoke with twelve individuals including Elders, mental health staff and practitioners, among others, who work from different vantage points in federal corrections, including at federal Healing Lodges and Indigenous community organizations. We also reviewed multiple interviews conducted as a part of other systemic investigations included in this report where issues related to CSC’s delivery of mental health services to incarcerated Indigenous peoples were raised. Together they all shared with us some of the key challenges experienced by both Indigenous individuals serving federal sentences, as well as those working in the system, in accessing and providing effective services and care. Further to this review, the following themes were identified:
- Discrimination and unconscious bias in mental health care create unique challenges for Indigenous prisoners.
- Availability and access to culturally-informed and trauma-informed mental health services for Indigenous peoples are lacking.
- Continuity of mental health care for Indigenous peoples upon release to the community setting is poor.
- Decolonization of mental health care in the prison system is required to achieve equity for Indigenous peoples serving federal sentences.
Findings
Discrimination and Unconscious Bias in Mental Health Care Create Unique Challenges for Indigenous Prisoners
Anti-Indigenous discrimination and bias exist in broader society and the health care system, and in turn, the correctional system. Numerous studies have found that individuals who experience racism have poorer mental and physical health outcomes.121 As numerous reports, commissions, and inquiries have demonstrated and documented, systemic discrimination occurs at all junctures of the criminal justice system, including corrections.122 For example, it is widely known that Indigenous peoples are more often targeted by police, have more contact with the courts, are often seen as less worthy victims by the police, more often have their credibility questioned, and their requests for assistance ignored. As this Office has reported previously, discrimination in the federal correctional setting can take many forms and materializes in the over-representation of Indigenous men and women, in custody settings generally, maximum security settings, Structured Intervention Unit (SIU) placements, and use of force incidents, to name a few. It can be seen in how Indigenous peoples are overwhelmingly assessed as higher risk and higher security compared to their non-Indigenous counterparts, they serve longer portions of their sentence, and have higher rates of revocation and recidivism, and among other indicators and outcomes. The consequences of such are that Indigenous peoples have less access to services, programs, and sources of support for their mental health needs and are serving their sentences in conditions that are not only inconsistent with wellbeing and healing but can serve to exacerbate symptoms and illness (e.g., isolation, volatile environments).
Discrimination and bias, as pertaining to mental health care for Indigenous prisoners, manifests in various ways, and can be seen at the micro and macro levels of mental health care in the prison setting. It can be seen in the manner in which mental health needs are screened and assessed at intake, to the daily interactions with staff, to the clinical decisions rendered by health care providers, to how mental health care is defined, legislated, governed, and implemented at a systems-level. In our review of the literature and in our conversations with individuals working in the correctional system, we observed that discrimination and bias (both conscious and unconscious) is a significant barrier to proper and humane patient care and has major impacts on Indigenous patient health. Recognizing that bias exists in the general health care system, the sources of discrimination are deep, structural, and intersectional between both race and the “inmate” status of patients in the prison system. While it is important to note that there are many mental health care providers within the federal correctional system working tirelessly, creatively, and collaboratively to provide quality care for Indigenous patients, it is also a devastating reality that there remain many potent sources of discrimination and bias that have negative impacts on Indigenous prisoners and their wellbeing. This is a source of frustration with patients and health care providers alike. Examples of these forms and sources of discrimination and bias in the prison system include the following:
Stereotyping and Stigma
Stereotyping and stigma associated with Indigenous peoples creates for an unwelcoming and at times hostile environment for Indigenous prisoners, making them less likely to seek mental health care. Stereotyping can include prejudiced beliefs perpetuated more broadly in society, that are held by health care providers, which in turn impacts the manner in which they engage with Indigenous patients. We have heard that stereotyping and stigma can include expressions of the false beliefs that Indigenous peoples do not know how to care for their own health, make poor lifestyle decisions, or utilize emotional distress and trauma as a ruse to obtain drugs and medications. As one Elder told us, “In order for Indigenous folks to access or seek mental help services, they have to trust they will be treated equally, like everyone else and not be viewed as seeking meds to get high.” These forms of prejudice, among many others, have significant negative impacts on clinical decision- making, and furthermore, discourage Indigenous peoples from seeking supports, out of the legitimate fear of being judged, shamed, mistreated, or turned away. Consequently, this serves to exacerbate the existing mental health issues of individuals and further entrench a lack of trust in health care providers. Given that mental health is closely tied to experiences of racism, exclusion, and isolation, these barriers also contribute to the onset of new mental health issues or sources of distress or illness.
Over-Reliance on Western Approaches to Mental Health Care
Organizational approaches to mental health care have been overly rigid and over-reliant upon Western approaches to mental health diagnosis, treatment, and the medical model. These models often ignore approaches that are Indigenous-led and conceptualized using a more holistic understanding of mental health and wellness. In some cases where Western approaches have been tailored to include Indigenous components or features, they are often “add-ons” or tweaks to existing approaches, simply adding a culturally-informed veneer. We also heard that a poor understanding of holistic conceptualizations of mental health treatment and programming has resulted in, for example, the loss of funding to Indigenous programs that serve to support mental health and wellbeing outside of the mainstream approaches. One staff member described the following situation: “As Indigenous people we don’t just look at mental, we look at emotional, spiritual, and physical…so when Elders are working with them, they’re able to deal with those elements. We have pipe ceremony, spirit baths, and we try to engage women in their culture. …We built a traditional sea going canoe... what we’ve seen with land-based healing – there’s a lot of change and healing that occurs. It’s a 4-day retreat. After the teachings, they would ride the canoe. Then they’d go into sweat lodge and a sharing circle, then feast and a closing circle. Unfortunately, when the cuts came, that was one of the first to go. Why would you cut Indigenous programs first considering the over-representation? If you’re trying to lower the number of Indigenous people inside, cutting cultural services is not going to help. I feel like we’re begging for money for our cultural/ spiritual pieces.”
Bias in Screening and Assessments
As has been reported by our Office previously, assessments and tools that screen for individual needs, including mental health, do not properly consider the social determinants of health and the root causes of mental health concerns for Indigenous peoples. These tools often reinforce stereotypes, blaming individuals for the consequences of colonial forces of oppression that have created the context in which mental health care and wellness are negatively affected. The bias in these tools results in the misidentification of needs, and the exclusion of more relevant needs, which in turn results in improper diagnosis and substandard care. While CSC collects and records information on Indigenous Social History (ISH) factors and mental health, neither of these sources of information appear to be used in consistent practice to inform decision-making about an individual’s case management and care. We have heard the recording of ISH information as a “copy and pasting” exercise, where information is recorded but not used. A recent report produced by the Service notes the following regarding ISH and mental health information: “…factors were frequently mentioned but not linked to the decision or recommendation, including mental health, family and community history of suicide...”.123 Staff lack the proper training to understand how to use ISH information in practice to inform decision-making and action. The social determinants of health, including ISH factors, are potent sources of information on the underlying causes of symptoms measured through assessment tools. Focusing on the assessment and treatment of symptoms alone, and ignoring root causes, not only serves to perpetuate discrimination of Indigenous peoples, it results in improper and ineffective care.
Lack of Indigenous Representation Among Health Care Staff Results in Low Cultural Competence of the System
As this Office has previously reported, the lack of Indigenous representation among health care staff and service providers within the prison system results in low levels of cultural competence and awareness among those interacting with Indigenous prisoners on a daily basis. Furthermore, staff training on cultural “awareness” has been described as inadequate, doing little to increase an often surface-level understanding among staff of Indigenous history, culture, and ways of knowing. A lack of Indigenous representation among mental health care and wellness providers, including the inadequate availability of Elders, results in few individuals who have the lived experience and knowledge of the needs of Indigenous peoples. Inadequate representation and cultural credentials among staff result in a poor understanding of the needs of Indigenous peoples and the most effective and relevant ways to support holistic wellbeing. This places an overwhelming burden on Indigenous patients to have to educate staff, look past their lack of knowledge, or avoid interactions with health care staff altogether. One individual we interviewed described the consequences as follows, “The lack of knowledge [of staff] perpetuates the trauma suffered by the Indigenous population.”
Availability and Access to Culturally-Informed and Trauma-Informed Mental Health Services for Indigenous Peoples are Lacking
As has been illustrated through the various investigations in this report, it is clear that many of the gaps and challenges in the broader Canadian health care system are reflected in the prison system. Among these gaps are adequate trauma-informed and culturally-informed services, supports, practitioners, and practices. As has been described, Indigenous individuals enter the correctional system with disproportionately high mental health needs, among other social determinants of health. This requires specialized care founded in the knowledge, context, and awareness of the socio- historical trauma experienced by individuals and groups, and the cultural realities that have impacts on how mental health and wellness may be differentially conceptualized, embodied, and treated. Consistent with a broader lack of trauma services, there are few Indigenous practitioners (e.g., psychologists, psychiatrists, nurses, social workers, Elders, Spiritual Caregivers, program providers) available to Indigenous individuals serving federal sentences. Furthermore, the various barriers Indigenous peoples face while behind bars, make accessing the few trauma-informed and culturally-informed care options, very difficult. For example, as reported in our Office’s investigation, Ten Years since Spirit Matters, access to Healing Lodges, which were established to be trauma and culturally-informed centres where corrections could be administered by and for Indigenous peoples, is only accessible to a small fraction (approximately 6%) of the Indigenous population, and largely only for those nearing the end of their sentence. Access to Elders and service providers who have the lived experience and the requisite knowledge to understand and treat the needs of individuals are few and far between .
In addition to the lack of availability, another significant barrier is the criteria for access to services. As one staff member put it: “Part of the problem is [the lack of] trauma-informed counselling. You have to meet high criteria to get psychological counselling. Group counselling isn’t great for trauma.” The lack and inaccessibility of effective mental health services for Indigenous prisoners often means that existing issues go undiagnosed, untreated, and in many cases worsen, and proliferate, due to the re-traumatizing experience of incarceration. This means that many of these individuals will reach the end of their sentence or be released without the tools, resources, and supports in place to successfully transition to a community setting.
Continuity of Mental Health Care for Indigenous Peoples Upon Release to the Community Setting is Poor
As described earlier in this report through the investigation into community discharge planning, the lack of mental health services within the prison system is a gap that continues when individuals are released into the community. The challenges stemming from this discontinuity are compounded for Indigenous individuals. Many Indigenous individuals face the challenges of navigating community reintegration pressures, meeting community supervision requirements, while in many cases struggling to manage mental health conditions. A small proportion of Indigenous individuals with mental health needs are released to the community with a clinical discharge plan, meaning few are provided with a release plan that adequately considers how mental health needs may amplify challenges that come along with complying with release conditions, securing housing and employment, and just meeting their basic daily needs.
For Indigenous individuals specifically, there are very few options for specialized Indigenous community-based residential facilities (i.e., halfway houses) which offer a more culturally conducive environment, and fewer yet that accept individuals dealing with mental health challenges. This creates difficulties not only for Indigenous individuals seeking a better environment upon release, but also puts pressure on the existing Indigenous CRFs to accept a wider variety and complexity of residents. As one Indigenous CRF staff member explained, “We sometimes take folks who are not accepted elsewhere, high risk, high need. But I find that who they are on paper is not who they are here. When they get here, it’s more like a home life and their defences go down and behaviours improve.” One community staff member with whom we spoke described the unique challenges for Indigenous women upon release, particularly those released to urban settings far from their home communities, “There’s a lot of borderline personality disorders, ADHD, a lot of depression. With women, there’s lots more self- harming, sometimes quite significant self-harming. More women with suicidal ideation and many of these women are care givers at the same time. Lots of Indigenous women with mental health issues who are far from their supports.” Individuals we interviewed also raised the growing need for specialized detox services for Indigenous peoples going to the community as a major challenge for reintegration, where there are simply not enough coordinated services to support these individuals and their health needs.
While the law provides for a mechanism of release planning that is done in collaboration with Indigenous communities or organizations to better meet the reintegration needs of Indigenous peoples (i.e., Section 84 releases), in reality, very few Section 84 releases are done.124 One individual that we spoke with, who received a Section 84 release plan expressed concern over those who did not get to benefit from that option: “These other guys [pauses]…, I feel bad. They don’t have that kind of support. They have no one to follow-up with, they don’t have a court order to take their meds or see a psychiatrist.” Gaps in release planning, lack of availability of Indigenous services in the community, and inadequate use of mechanisms afforded to the Service by law (e.g., Healing Lodges and Section 84 releases) all contribute to the inadequacy of mental health care for Indigenous peoples who need these supports for a successful return to the community.
Decolonization of Mental Health Care in the Prison System is Required in Order to Achieve Equity for Indigenous Peoples Serving Federal Sentences
In 2015, the Truth and Reconciliation Commission (TRC) identified fundamental and structural deficiencies in the Canadian health care system, including mental health care for those serving federal sentences, as areas requiring significant change to advance reconciliation. Many, if not all these deficiencies, as far as the federal prison system is concerned, remain today. Further to the TRC’s findings, the commission put forward calls-to-action to improve the provision of health care for Indigenous peoples, which included the following:
- Close the gap in health outcomes for Indigenous Peoples
- Support traditional healing practices
- Increase the number of Indigenous Peoples in the health professions
- Integrate cultural safety into health systems
- Improve supports for Indigenous patients
The following year, in 2016, the United Declaration on the Rights of Indigenous Peoples (UNDRIP) was fully endorsed by Canada. The United Nations Declaration on the Rights of Indigenous Peoples Act (the UN Declaration Act) was later introduced in Parliament and received Royal Assent in 2021. The UN Declaration Act requires the government to consult and co-operate with Indigenous peoples to ensure that federal laws are consistent with the Declaration. One of the Government of Canada’s commitments appears to be to ensure meaningful participation of Indigenous Peoples in decisions that affect them and their communities. It is reasonable to assume that this includes being actively involved in the development of social institutions such as health and justice, traditional medicines and health care practices, and access to the highest quality of mental health.125 Most recently, on March 11, 2025, the federal government released its much-anticipated Indigenous Justice Strategy. Among many other notable areas identified, the mental health of Indigenous peoples in the criminal justice system is included as a priority area requiring action (e.g., Action item #17 and sections 2.1 and 2.6 on Inuit Wellness), much as it was when it was a decade early in the TRC calls-to-action.
As this Office has reported previously, the problems are well-known and documented and the action plans have been developed. As articulated in the TRC, among other reports, the UNDRIP, and now the Indigenous Justice Strategy report, Corrections has a lot of work to do to meet the health care needs of Indigenous peoples in their care. And while federal corrections has developed its own set of plans, most recently an Indigenous Wellness Action Plan, there are clearly still considerable practical and fundamental changes required to address the issues within the correctional mental health care system. The prison system is an inherently colonial institution. Given this reality, the infusion of new programs and services can only go so far in changing the prevailing norms, culture, and ethos underlying current policy and practice. Changing how the prison system acknowledges and addresses the needs of Indigenous individuals under their custody and care requires greater efforts toward a systemic decolonization of the prison health care system, from top to bottom. The CSC is ill-equipped to address the many concerns raised in this investigation, and more resources to improve the capacity of CSC to better respond to the mental health and wellness needs of Indigenous peoples will continue to fail or only have marginal positive results. It is clear that the most effective way for CSC to move forward is to reallocate a significant portion of its budget to fund new community-run Healing Lodges, support a greater number of Section 84 releases, and invest in Indigenous communities and organizations to deliver holistic, culturally-responsive mental health and wellness services. This equitable reallocation will support CSC and the Government of Canada’s many commitments to ensure in concrete actions the implementation of reconciliation, self-government, and self-determination of Indigenous peoples.
- I recommend that CSC reallocate a significant portion of its resources to funding additional section 81 healing lodges and increase funding of existing section 81 healing lodges within the 2025-26 fiscal year, to enable them to provide authentic, Indigenous-led, holistic mental health and wellness services that better meet the needs of Indigenous individuals with mental health issues, in ways that are culturally- and trauma-informed, and free of discrimination and unconscious bias.
CSC's Response: ACCEPTED IN-PRINCIPLE
CSC provides funding to Section 81 healing lodges through a negotiated process that considers individual community needs. While funding is guided by demand and utilization, additional resources may be allocated as required to support specific priorities.
To enhance the effectiveness and sustainability of Section 81 agreements, CSC is taking concrete steps to improve funding flexibility, support Indigenous-led innovation, and ensure alignment with community needs. These next steps aim to reinforce partnerships, promote culturally responsive services, and modernize funding approaches.
Next Steps:
- Explore options for supplementary funding of new and existing agreements, while ensuring internal resources are available to support implementation when needed.
- Support innovative approaches that advance community-led justice and strengthen the role of self-governing Indigenous governments.
- Formalize opportunities for supplementary funding to expand Indigenous led mental health/health supports/services during (re)negotiation of S81 agreements.
- Ensure requests for additional funding from existing Section 81 partners with current agreements are considered accordingly.
- Modernize the funding models available to s.81 Partners to ensure operational needs are met. (Completed)
Timeline: Ongoing. Given that all the deliverables are ongoing and/or based on interest and negotiations with both current and potential section 81 partners, the implementation timeline will also be ongoing.
Correctional Investigator’s Outlook for 2025-26
As my tenure as Canada’s Correctional Investigator draws to a close in 2026, I find myself reflecting with pride on nine years of meaningful progress and transformation as CI. It has been a profound honour to lead this Office through a period of significant evolution, one marked by a deepened commitment to rigour, accountability, and principled oversight.
Over the past nine years, we have fundamentally strengthened the way the Office of the Correctional Investigator conducts its work. With new funding secured in both 2018 and 2023, we were able to expand our capacity and sharpen our focus. These investments allowed us to streamline and enhance our early resolution function, stabilize our investigative team, and shift toward more proactive, inspection-style visits, bringing our practices in line with international standards for effective prison oversight.
These enhancements have not only improved the quality and reach of our systemic investigations, but also enabled us to align more closely with our corporate priorities. By building diverse, multidisciplinary teams of investigators and analysts, we have fostered greater staff safety, deepened subject-matter expertise, and ensured that those responding to complaints reflect the diversity of the populations we serve.
Through the tireless dedication of our staff, the Office has earned and solidified its reputation, both domestically and internationally, as a model of excellence in correctional oversight. I was privileged to serve as Chair of the International Corrections and Prisons Association’s (ICPA) External Prison Oversight and Human Rights Network, a global forum for sharing best practices and advancing transparency in corrections. I was deeply honoured to receive the ICPA’s 2023 Head of Service Award, a recognition that affirms the impact of our work and the strength of our commitment to humane, professional corrections.
Looking ahead, the Office is exceptionally well-positioned for the future. It is well-resourced, internationally respected, and grounded in a culture of continuous improvement. As we prepare for a leadership transition, the organization stands ready to embrace new opportunities while remaining steadfast in its mission. The coming year will be both reflective and forward-looking, as we revisit past recommendations that have been put forward by the Office over the last decade and identify recommendations that remain pressing yet unaddressed.
In closing, it has been the privilege of a lifetime to serve in this role. I leave behind an Office that is strong, principled, and prepared for the future—a legacy built on sound ombudsmanship and a deep commitment to social justice and human rights. I am confident that under new leadership, the Office of the Correctional Investigator will continue to thrive and lead with integrity, compassion, and resolve.
Ed McIsaac Human Rights in Corrections Award
The Ed McIsaac Human Rights in Corrections Award was established in December 2008, in honour of Mr. Ed McIsaac, long-time Executive Director of the Office of the Correctional Investigator and strong promoter and defender of human rights in federal corrections. It commemorates outstanding achievement and commitments to improving corrections in Canada and protecting the human rights of incarcerated persons.
The 2024 recipient of the Ed McIsaac Award was Michel Gagnon. For more than 30 years, Mr. Gagnon served as Executive Director of Maison Cross Roads in Montréal, Quebec, a not-for-profit community-based organization that provides social and community reintegration programs and services to people who come into conflict with the law. Mr. Gagnon has devoted much of his career to spearheading support services to meet the growing and unique needs of individuals serving life sentences as well as the aging correctional population. These include Service Oxygène in Quebec and the LifeLine program .
ANNEX A: Summary of Recommendations
- I recommend that CSC’s RTCs be redefined and formally recognized as Intermediate Mental Health Care facilities, with limited capacity to manage emergency psychiatric cases. Individuals diagnosed with serious mental illness—those experiencing acute psychiatric crises, persistent suicidal ideation, or chronic self-harming behaviours requiring long-term psychiatric care—should be transferred to community-based psychiatric hospitals better suited to meet their needs.
- I recommend that the Government of Canada/Minister of Public Safety reconsider its recent $1.3 billion investment in a replacement facility for RTC Atlantic (Shepody). Instead, efforts and funding should be redirected to support CSC in reallocating its current resources toward facilitating the transfer of individuals with serious mental illness to provincial psychiatric hospitals. This includes supporting the creation or expansion of bed space in provinces facing capacity constraints.
I recommend that once the RTCs are reprofiled as Intermediate Mental Health Care facilities:
CSC work with mental health professionals to see how the current RTC infrastructure could be significantly improved and become more therapeutic, including the use of paint, plants, grass in yards, benches, carpets, posters, and sofas where security concerns could be mitigated.
The Minister of Public Safety immediately review and assess release options (e.g., medical and/or geriatric parole) for older and long-serving patients who do not pose undue risk to public safety, advance legislative amendments to the CCRA, accordingly. CSC should actively invest in community corrections to create bedspace in long-term, hospice and retirement home settings, with a target of 200 beds in five years.
CSC develop a policy specific to the governance and operation of the RTCs, in consultation with external experienced mental health professionals from its inception.
CSC review the implementation of the Engagement and Intervention Model with a particular focus on its application with those suffering from mental health conditions. CSC should also cease the use of inflammatory sprays as a first response to incidents of self-harm, in favour of health care-driven, de-escalation and therapeutic responses and techniques.
CSC develop a governance model for RTCs, similar to that of external community forensic psychiatric facilities, including an autonomous reporting and governance structure so that all matters related to health, from separate staffing rosters to training of staff, to complete and unfettered control over budgets and resources, are decided by clinicians, not Wardens or operational staff.
CSC develop training, onboarding, policies, procedures, and directives specific to the function and purpose of RTCs and the welfare of patients.
CSC develop a specific mandate and mission statement that reflects the purpose, goals, and methodology around which staff across disciplines can collectively unify their efforts to achieve a common goal.
CSC develop practices to ensure that the NBOI process balances investigation of compliance-driven issues with issues of quality, nature, and frequency of interventions provided to individuals with mental health concerns, including treating these reports as consistent, service-wide, learning and knowledge mobilization tools, in order to prevent further deaths and serious injury.
CSC immediately introduce, at a minimum, one Patient Advocate in each RTC to support patient-centred care and provide legitimately independent advocacy for patients in navigating the medical system in a correctional context.
I recommend that CSC, in close partnership with external, community organizations with expertise on cognitive deficits:
Review and update Guideline 800-10: Intellectual Disability and the Mental Health Guidelines to provide more comprehensive policy and guidelines for the management and supervision of individuals with cognitive deficits by the end of fiscal year 2025-2026. This must be conducted in consultation with institutional staff who deal with these issues on a daily basis.
Identify and implement a consistent, comprehensive, timely and standardized approach to the screening and assessment of individuals with cognitive deficits.
Ensure that adapted correctional programming is made available at all sites, that program facilitators receive the appropriate training to deliver adapted programs, and that the threshold for admission to adapted programs be adjusted to allow for more participants.
Develop and implement new mandatory training on working with individuals with cognitive deficits in a correctional environment for all staff by 2026-2027. This should include more comprehensive and applied materials for correctional officer training.
I recommend that CSC double the budget allocation to community-based residential facilities, CCCs, and community mental health services, over the next five fiscal years, to meet the changing mental health profile of parolees; appropriately compensate external partners and service providers; and, ensure that community mental health and transitional services are resourced adequately.
I recommend that CSC implement changes to Discharge Planning and Community Mental Health by the end of fiscal 2025-2026, including the following enhancements:
Update and streamline national policies and tools, including clear service standards and reporting requirements;
Implement a mental health needs assessment that enables reintegration planning;
Improve training, education, policies, and procedures around information sharing;
Ensure compliance with policies around releasing individuals with government identification (preferably birth certificates); and,
Remove barriers to accessing government funded health and mental health care on release by focusing on improving collaboration with provincial and territorial health authorities as well as community partners.
I recommend that CSC immediately respond to the recommendation and issues previously raised by the OCI regarding Therapeutic Ranges and the provision of intermediate mental health care.
I recommend that CSC immediately respond to and action each of the 38 recommendations outlined in the IMHC Working Group report titled, “Review of Intermediate Mental Health Care Services in Correctional Service Canada Mainstream Institutions and Associated Recommendations” (January 11, 2023). Specifically, I recommend that CSC:
Develop and publicly report on a plan addressing and responding to each of the 38 recommendations individually with concrete actions and timelines by the end of fiscal year 2025-2026.
Ensure complete implementation of each of the 38 recommendations by 2026-2027.
I recommend that CSC works closely with an external, expert mental health organization to develop an evidence-based, comprehensive strategy for trauma-informed services and trauma-specific treatment for federally sentenced women. This strategy should include:
Standardized screening for trauma, victimization, and Adverse Childhood Experiences (ACEs);
Implementation of trauma-informed practices across CSC policies and procedures, supported by specialized staff training;
Access to gender- and culturally-responsive trauma-specific therapy and counselling; and,
Safe, supportive environments for women to begin the healing process.
The new strategy should be fully implemented by June 2026. The new model should then be evaluated by CSC, and a similar approach extended to male institutions nationwide.
I recommend that CSC reallocate a significant portion of its resources to funding additional section 81 healing lodges and increase funding of existing section 81 healing lodges within the 2025-26 fiscal year, to enable them to provide authentic, Indigenous-led, holistic mental health and wellness services that better meet the needs of Indigenous individuals with mental health issues, in ways that are culturally- and trauma-informed, and free of discrimination and unconscious bias.
ANNEX B: Annual Statistics
COMPLAINTS
Table A. Total Complaints
| Active | Addressed | Grand Total | |
|---|---|---|---|
| Total Complaints126 | 346 | 4,006 | 4,352 |
Top Five Most-Frequently Identified Complaint Categories Overall and by Priority Populations
| Population and Complaint Category | # | % |
|---|---|---|
| Overall | 4,352 | |
| Complaint Category | ||
| Conditions of Confinement | 480 | 11.0% |
| Health Care | 458 | 10.5% |
| Staff | 440 | 10.1% |
| Cell Effects | 317 | 7.3% |
| Transfer | 273 | 6.3% |
| Indigenous | 1,200 | |
| Complaint Category | ||
| Health Care | 137 | 11.4% |
| Staff | 117 | 9.8% |
| Conditions of Confinement | 112 | 9.3% |
| Cell Effects | 89 | 7.4% |
| Transfer | 82 | 6.8% |
| Women | 472 | |
| Complaint Category | ||
| Conditions of Confinement | 85 | 18.0% |
| Health Care | 58 | 12.3% |
| Staff | 52 | 11.0% |
| Conditional Release | 21 | 4.4% |
| Cell Effects | 19 | 4.0% |
Table B. Complaints, Individual Complainants, and In-Custody Population by Region
| Region | Complaints | Individuals127 | In-Custody Population128 |
|---|---|---|---|
| Atlantic | 442 | 211 | 1,326 |
| Quebec | 1,065 | 525 | 3,244 |
| Ontario | 819 | 433 | 4,138 |
| Prairies | 930 | 535 | 4,272 |
| Pacific | 621 | 300 | 1,857 |
| Total129 | 3,877 | 2,004 | 14,837 |
Table C. Individual Complainants and Complaints by Facility Type
| Facility Type | Complaints | Individuals |
|---|---|---|
| Institutions for Men | 3,253 | 1,687 |
| Multi-Level | 1,136 | 648 |
| Maximum130 | 957 | 382 |
| Medium | 1,147 | 647 |
| Minimum | 13 | 10 |
| Institutions for Women | 442 | 231 |
| Treatment Centres | 147 | 65 |
| Healing Lodges | 35 | 21 |
| CCC-CRF131 | 161 | 108 |
| Community | 71 | 51 |
| Grand Total132 | 4,109 | 2,163 |
Table D. OCI Complaints by Category and Resolution Status133
| Complaint Category | Active | Addressed | Grand Total |
|---|---|---|---|
| Case Preparation | 1 | 27 | 28 |
| Cell Effects | 17 | 300 | 317 |
| Cell Placement | 3 | 94 | 97 |
| Claims Against the Crown | 1 | 27 | 28 |
| Community Supervision | 2 | 5 | 7 |
| Conditional Release | 4 | 130 | 134 |
| Conditions of Confinement | 47 | 433 | 480 |
| Death of Inmate | 3 | 6 | 9 |
| Diets | 4 | 42 | 46 |
| Discipline | 4 | 40 | 44 |
| Discrimination | 5 | 36 | 41 |
| Employment | 6 | 59 | 65 |
| File Information | 9 | 93 | 102 |
| Financial Matters | 7 | 112 | 119 |
| Food Services | 6 | 46 | 52 |
| Grievance | 4 | 85 | 89 |
| Harassment by Inmate | 7 | 22 | 29 |
| Harm Reduction | 0 | 6 | 6 |
| Health and Safety (of worksite conditions) | 3 | 18 | 21 |
| Health Care | 33 | 425 | 458 |
| Independent External Decision Maker | 0 | 3 | 3 |
| Inmate Request Process | 11 | 111 | 122 |
| Legal Access | 5 | 70 | 75 |
| 7 | 51 | 58 | |
| Mental Health | 5 | 64 | 69 |
| Mother-Child Program | 1 | 3 | 4 |
| Office of the Correctional Investigator134 | 6 | 100 | 106 |
| Official Languages | 1 | 4 | 5 |
| Outside Jurisdiction | 4 | 144 | 148 |
| Programs | 8 | 41 | 49 |
| Release Procedures | 2 | 16 | 18 |
| Safety/Security | 12 | 104 | 116 |
| Search | 3 | 36 | 39 |
| Security Classification | 19 | 96 | 115 |
| Sentence Administration | 2 | 18 | 20 |
| Serious Injury of Inmate | 0 | 3 | 3 |
| Special Handling Unit-National Advisory Reviews | 0 | 1 | 1 |
| Spiritual or Religious | 3 | 15 | 18 |
| Staff | 21 | 419 | 440 |
| Structured Intervention Unit (SIU) | 7 | 55 | 62 |
| Telephone | 5 | 74 | 79 |
| Temporary Absence | 5 | 60 | 65 |
| Transfer | 22 | 251 | 273 |
| Urinalysis | 0 | 17 | 17 |
| Use of Force | 10 | 45 | 55 |
| Visits | 17 | 146 | 163 |
| Not Enough Information to Categorize | 4 | 53 | 57 |
| Total | 346 | 4,006 | 4,352 |
Table E. Complainants and Complaints by Self-Reported Ethnicity
| Women | Men | |||
|---|---|---|---|---|
| Ethnicity | Complaints | Individuals | Complaints | Individuals |
| White | 237 | 129 | 1,629 | 891 |
| Indigenous | 172 | 96 | 1,028 | 569 |
| Black | 28 | 12 | 570 | 237 |
| Other Visible Minority, Multi-Ethnic, or Unspecified | 35 | 22 | 411 | 208 |
| Total135 | 472 | 259 | 3,638 | 1,905 |
Table F. Disposition of Cases
| Action136 | # |
|---|---|
| Internal Resolution | 2,349 |
| Investigation | 2,621 |
| Total | 4,970137 |
REVIEWS
Table G. Mandated Reviews138 by Type of Incident (2024-25)
| Incident Type | Reviews |
|---|---|
| Assault | 98 |
| Overdose Interrupted | 20 |
| Attempted Suicide | 15 |
| Suicide | 14 |
| Homicide | 11 |
| Overdoses | 9 |
| Death (Natural Cause)139 | 5 |
| Self-Injury | 5 |
| Use of Force | 3 |
| Accidental Injuries | 1 |
| Total | 181 |
Use of Force Reviews Conducted by the OCI in 2024-25
The Correctional Service of Canada provides the Office with a use of force package for each case, which typically includes: a use of force report; the incident video; the Health Services use of force checklist; a post-incident checklist; the officer’s statement or Observation Report; and, an action plan to address deficiencies. OCI use of force review analysts then triage each use of force package to determine whether a summary or full review is required.140 In 2024-25, there was a total of:
- 2,367 unique use of force cases.
-
578 use of force cases processed by the OCI use of force review analysts.
- 338 cases were triaged by the OCI, but only required a summary review.
- 240 cases received a full review by the OCI’s use of force analysts.
Table H. Use of Force Reviews Conducted by the OCI in 2024-25
| Region | Summary Review | Full Review | Total |
|---|---|---|---|
| Atlantic | 32 | 30 | 62 |
| Quebec | 104 | 54 | 158 |
| Ontario | 81 | 58 | 139 |
| Prairies | 86 | 83 | 169 |
| Pacific | 35 | 15 | 50 |
| Total | 338 | 240 | 578 |
VISITS
Table I. Interactions, Interviews, and Visits Conducted by the OCI by Region and Facility (2024-25)
| Region / Facility | Interactions141 | Interviews142 |
OCI Days in Facilities143 |
Person Days in Facilities144 |
|---|---|---|---|---|
| Atlantic | 394 | 145 | 27 | 39 |
| Atlantic | 164 | 61 | 9 | 12 |
| Dorchester | 74 | 22 | 5 | 5 |
| Nova Institution for Women | 72 | 49 | 6 | 9 |
| Shepody Healing Centre | 10 | 0 | 3 | 9 |
| Springhill | 47 | 13 | 4 | 4 |
| CCC-CRF | 17 | 0 | 0 | 0 |
| Community | 10 | 0 | 0 | 0 |
| Quebec | 1,046 | 432 | 81 | 123 |
| Archambault | 168 | 29145 | 8 | 13 |
| Cowansville | 63 | 45 | 8 | 16 |
| Regional Reception Centre | 136 | 45 | 10 | 11 |
| Donnacona | 82 | 60 | 12 | 21 |
| Drummond | 71 | 63 | 8 | 9 |
| Federal Training Centre | 129 | 53 | 9 | 17 |
| Joliette | 69 | 41 | 6 | 9 |
| La Macaza | 78 | 36 | 6 | 6 |
| Port-Cartier | 117 | 60 | 10 | 13 |
| Special Handling Unit (SHU) | 60 | 0 | 0 | 0 |
| Institut Philippe-Pinel de Montréal | 0 | 0 | 1 | 2 |
| CCC-CRF | 52 | 0 | 3 | 6 |
| Community | 21 | 0 | 0 | 0 |
| Ontario | 871 | 287 | 54 | 92 |
| Bath | 95 | 17146 | 5 | 6 |
| Beaver Creek | 90 | 39 | 6 | 12 |
| Collins Bay | 60 | 35 | 6 | 9 |
| Grand Valley Institution for Women | 95 | 59 | 6 | 9 |
| Joyceville | 73 | 45147 | 6 | 6 |
| Millhaven | 228 | 52148 | 11 | 26 |
| Warkworth | 122 | 40 | 7 | 11 |
| CCC-CRF | 65 | 0 | 4 | 7 |
| Community | 43 | 0 | 3 | 6 |
| Prairies | 886 | 305 | 52 | 95 |
| Bowden | 117 | 35 | 6 | 12 |
| Buffalo Sage Wellness House | 5 | 2 | 1 | 2 |
| Drumheller | 123 | 55 | 6 | 12 |
| Eagle Women’s Lodge | 1 | 0 | 0 | 0 |
| Edmonton | 97 | 46 | 9 | 12 |
|
Edmonton Institution for Women |
51 | 37 | 6 | 9 |
| Grande Cache | 77 | 47 | 6 | 9 |
| Grierson | 3 | 0 | 0 | 0 |
| Okimaw Ohci Healing Lodge | 6 | 0 | 0 | 0 |
| Pê Sâkâstêw Centre | 7 | 6 | 1 | 2 |
| Regional Psychiatric Centre | 60 | 0 | 3 | 12 |
| Saskatchewan | 201 | 55 | 6 | 12 |
| Stan Daniels Healing Centre | 8 | 2 | 1 | 2 |
| Stony Mountain | 87 | 20 | 4 | 5 |
| Willow Cree Healing Lodge | 3 | 0 | 0 | 0 |
| CCC-CRF | 27 | 0 | 2 | 4 |
| Community | 13 | 0 | 1 | 2 |
| Pacific | 561 | 214 | 40 | 84 |
|
Fraser Valley Institution for Women |
43 | 50 | 8 | 16 |
| Kent | 147 | 40 | 6 | 12 |
|
Kwìkwèxwelhp Healing Village |
6 | 0 | 0 | 0 |
| Matsqui | 53 | 39 | 5 | 10 |
| Mission | 134 | 33 | 6 | 9 |
| Mountain | 69 | 45 | 3 | 6 |
| Pacific | 25 | 0 | 0 | 0 |
| Regional Reception Centre | 12 | 0 | 0 | 0 |
| Regional Treatment Centre | 30 | 7 | 6 | 19 |
| William Head | 10 | 0 | 0 | 0 |
| CCC-CRF | 23 | 0 | 4 | 8 |
| Community | 9 | 0 | 2 | 4 |
| Unspecified Institution149 | 108 | 0 | 0 | 0 |
| Grand Total | 3,866 | 1,383 | 254 | 433 |
Toll-Free Contacts in 2024-25
Federally sentenced individuals and members of the public can contact the OCI by calling our toll-free number (1-877-885-8848) anywhere in Canada. All communications between federally sentenced individuals and the OCI are confidential.
Number of toll-free contacts received in the reporting period: 16,739
Number of minutes recorded on toll-free line: 95,997
Footnotes
-
Footnote 1
-
The United Nations Standard Minimum Rule for the Treatment of Prisoners being referred to is #109(1): Persons who are found to be not criminally responsible, or who are later diagnosed with severe mental disabilities and/or health conditions, for whom staying in prison would mean an exacerbation of their condition, shall not be detained in prisons, and arrangements shall be made to transfer them to mental health facilities as soon as possible.
-
Footnote 2
-
According to CSC, this figure encompasses all projected expenses, including contingencies, allowances, escalation, and internal GoC fees and salaries, as well as taxes. It does not solely reflect the construction cost.
-
Footnote 3
-
In addition to the 38 beds at the Shepody Healing Centre, there are an additional 15 beds at Dorchester Penitentiary which are used by Shepody.
-
Footnote 4
-
In Ontario, a Schedule 1 facility is a designated psychiatric facility under the Mental Health Act.
-
Footnote 5
-
Health Standards Organization (2024). Correctional Health Services standard. HSO/CSC document provided to the OCI in February 2025.
-
Footnote 6
-
CSC (2024). Profile of Mental Health Care Patients. CSC Document provided to the OCI in October 2024.
-
Footnote 7
-
Office of the Correctional Investigator (OCI, 2009). 2008-2009 Annual Report; Mental Health and Drug and Alcohol Addition in the Federal Correctional System, OCI Appearance at the Standing Committee on Public Safety and National Security (SECU; December 2010).
-
Footnote 8
-
Office of the Correctional Investigator (OCI, 2018). 2017-2018 Annual Report; Bradford, J. (Dec. 2017). The regional treatment centres. Unpublished report.
-
Footnote 9
-
The St-Lawrence Valley Correctional and Treatment Centre in Brockville, ON; Institut national de psychiatrie légale Philippe-Pinel in Montréal, QC; The Forensic Psychiatric Hospital in Coquitlam, BC; The Canadian Association of Mental Health Secure Forensic Units in Toronto, ON
-
Footnote 10
-
Correctional Service Canada. (n.d.). Health Centre of Excellence. Government of Canada. https://www.canada.ca/en/correctional-service/corporate/facilities-security/health-centre-excellence.html.
-
Footnote 11
-
The United Nations Standard Minimum Rule being referred to is #109 (1): Persons who are found to be not criminally responsible, or who are later diagnosed with severe mental disabilities and/or health conditions, for whom staying in prison would mean an exacerbation of their condition, shall not be detained in prisons, and arrangements shall be made to transfer them to mental health facilities as soon as possible.
-
Footnote 12
-
Data retrieved from the Corporate Reporting System – Modernized (CRS-M) on March 9, 2025.
-
Footnote 13
-
Data retrieved from CSC’s Data Warehouse on March 9, 2024. Note: data captured for FY 2024-25 does not represent the entire year, given the date it was obtained.
-
Footnote 14
-
Office of the Correctional Investigator (2024). 2023-2024 Annual Report.
-
Footnote 15
-
Public Sector Integrity Commissioner. (2020). Findings of the Public Sector Integrity Commissioner in the matter of an investigation into a disclosure of wrongdoing: Correctional Service of Canada case report. Ottawa, Canada: Office of the Public Sector Integrity Commissioner of Canada.
-
Footnote 16
-
Ibid.
-
Footnote 17
-
Correctional Service Canada. (2021). Evaluation of the Engagement and Intervention Model: Summary. Government of Canada. https://www.canada.ca/en/correctional-service/corporate/transparency/evaluation-reports/engagement-intervention-model/engagement-intervention-model-summary.html
-
Footnote 18
-
All data for this section are for the period between April 1st 2024 and January 16th 2025.
-
Footnote 19
-
A Standing Order is a document created to operationalize a Commissioner’s Directive or Guidelines where there is a need to specify rules and processes unique to the operational unit.
-
Footnote 20
-
Union of Canadian Correctional Officers. (2025). Agreements. UCCO-SACC-CSN. https://ucco-sacc-csn.ca/agreements/.
-
Footnote 21
-
Note: The kimisinaw (Cree word for older sister) is specific to the Okimaw Ohci Healing Lodge.
-
Footnote 22
-
Correctional Service Canada. (2025). Testing for front-line jobs. Government of Canada. https://www.canada.ca/en/correctional-service/services/you-csc/working-csc/test-front-line-jobs.html.
-
Footnote 23
-
Incompatible offenders are identified when CSC believes there are reasonable grounds suggesting one offender poses a threat to the safety and wellbeing of another.
-
Footnote 24
-
OCI (2011). 2010-2011 Annual Report.
-
Footnote 25
-
Data retrieved from CSC’s Data Warehouse on March 9, 2025.
-
Footnote 26
-
Data retrieved from CSC’s Data Warehouse on March 9, 2025.
-
Footnote 27
-
OCI (2023). 2022-2023 Annual Report
-
Footnote 28
-
See the Case Study of a Death at RTC Millhaven in the 2023-2024 Annual Report
-
Footnote 29
-
The OCI recognizes that terminology in the domain of neurodiversity and cognitive disorders is evolving and there is no consensus on a single term that captures the heterogeneity of cognitive and intellectual needs. Unless otherwise specified, the broader term of ‘cognitive deficits’ and person-first language (e.g., persons with autism) will be used throughout this report. CSC documentation primarily uses the term ‘cognitive impairment’.
-
Footnote 30
-
Dodd, S., Doyle, C., Dickinson, H., et al., (2022). The forgotten prisoners: Exploring the impact of imprisonment on people with disability in Australia. Criminology & Criminal Justice, 24(2), 395-412; García-Largo, L. M., Martí-Agustí, G., Martin-Fumadó, C., et al., (2020). Intellectual disability rates among male prison inmates. International Journal of Law and Psychiatry, 70; Hellenbach, M., Karatzias, T., & Brown, M. (2017). Intellectual Disabilities Among Prisoners: Prevalence and Mental and Physical Health. Journal of Applied Research in Intellectual Disabilities, 230-241; Lin, E., et al., (2017). Intellectual and developmental disabilities and Ontario’s forensic inpatient system: A population-based cohort study. Psychology, Crime and Law, 23(9), 914–926.
-
Footnote 31
-
Billstedt, E., Anckarsäter, H., Wallinius, M., & Hofvander, B. (2017). Neurodevelopmental disorders in young violent offenders: Overlap and background characteristics. Psychiatry Research, 252, 234–241.; Hofvander, B., Bering, S., Tärnhäll, A., Wallinius, M., & Billstedt, E. (2019). Few differences in the externalizing and criminal history of young violent offenders with and without autism spectrum disorders. Frontiers in Psychiatry, 10, Article 911.
-
Footnote 32
-
Hunter, S., Kois, L. E., Peck, A. T., et al., (2023). The prevalence of traumatic brain injury (TBI) among people impacted by the criminal legal system: An updated meta-analysis and subgroup analyses. Law and Human Behavior, 47(5), 539–565.
-
Footnote 33
-
Popova, S., Lange, S., Bekmuradov, D., et al., (2011). Fetal Alcohol Spectrum Disorder Prevalence Estimates in Correctional Systems: A Systematic Literature review. Can J Public Health, 102(5), 336–340.
-
Footnote 34
-
Hellenbach, M., et al., (2017); Office of the Inspector of Custodial Services (OICS; 2021). Use of force against prisoners in Western Australia. OICS Government of Western Australia.
-
Footnote 35
-
Helverschou, S. B., Steindal, K., Nøttestad, J. A., et al., (2018). Autistic individuals in the criminal justice system: An examination of support structures and recidivism. Journal of Autism and Developmental Disorders, 48(5), 1820-1833; de Geus, E. Q. et al., (2021). Acquired brain injury and interventions in the offender population: A systematic review. Frontiers in Psychiatry, 12; Hellenbach, M., et al, (2017).
-
Footnote 36
-
Office of the Inspector of Custodial Services (OICS; 2024). People in custody with intellectual disabilities. OICS, Government of Western Australia.
-
Footnote 37
-
de Geus, E. Q., et al., (2021); Hunter S., et al., 2023.
-
Footnote 38
-
Dodd S., et al., (2022).
-
Footnote 39
-
Office of the Inspector of Custodial Services (OICS; 2024). People in custody with intellectual disabilities. OICS, Government of Western Australia.
-
Footnote 40
-
See the Employment and Social Development Canada Guidance on the Accessible Canada Regulations for further information on the distinction between what they define as learning disabilities and developmental disabilities (https://www.canada.ca/en/employment-social-development/programs/accessible-canada-regulations-guidance/consultation/key-concepts.html)
-
Footnote 41
-
Office of the Correctional Investigator (2019). Special Report on Aging and Dying in Prison: An Investigation into the Experience of Older Individuals in Federal Custody.
-
Footnote 42
-
The literature review was conducted in collaboration with the Centre for Addiction and Mental Health.
-
Footnote 43
-
This policy will be referred to as GL 800-10 throughout the remainder of this report.
-
Footnote 44
-
CSC Mental Health Guidelines (October 2023) outline the provision of mental health services to offenders in CSC mainstream institutions, regional treatment centres, and in the community.
-
Footnote 45
-
CSC documentation primarily uses the term ‘cognitive impairment’. According to the CSC Mental Health Guidelines (2023) The OMS Impairment Flag is activated when an individual is identified by a health care professional as having a cognitive impairment that may impact institutional functioning and/or require an adapted approach for case management and correctional planning.
-
Footnote 46
-
Stewart, L. A., Wilton, G., & Sapers, J. (2016). Offenders with cognitive deficits in a Canadian prison population: Prevalence, profile, and outcomes. International journal of law and psychiatry, 44, 7-14.
-
Footnote 47
-
GAMA is designed to evaluate intellectual ability and an individual’s overall general ability with items that require the application of reasoning and logic to solve problems.
-
Footnote 48
-
Domains of Functioning - Cognitive Functioning: involve cerebral functions that include reasoning, memory, attention, language, and lead to the attainment of knowledge. This domain may relate to intellectual disabilities, learning disabilities, dementia, and other related cognitive impairments.
-
Footnote 49
-
The Regional Psychiatric Facility, located in Saskatoon, SK, is the only CSC treatment centre that has a unit for women.
-
Footnote 50
-
Office of the Correctional Investigator (2024) 2023-2024 Annual Report
-
Footnote 51
-
Kerodal A.G., Akca, D., Jewell, L., et al., (2021) A Process Evaluation of the Regional Psychiatric Centre’s Fetal Alcohol Spectrum Disorder Pilot Project: Year 1 (July 2018-2019). Centre for Forensic Behavioural Science and Justice Studies, University of Saskatchewan.
-
Footnote 52
-
See Andrews & Bonta, 2024, The Psychology of Criminal Conduct (7th Ed) New York, NY: Routledge; Andrews, D. A., Zinger, I., Hoge, R. D., Bonta, J., Gendreau, P., & Cullen, F. T. (1990). Does correctional treatment work? A psychologically informed meta-analysis. Criminology, 28, 369-404.
-
Footnote 53
-
Adapted Integrated Correctional Program Model admission criteria (Information provided by CSC from a documentation request in December 2024).
-
Footnote 54
-
Screening Tool – Adapted ICPM (Information provided by CSC from a documentation request in December 2024).
-
Footnote 55
-
Stewart, L. A., Wilton, G., & Sapers, J. (2016). Offenders with cognitive deficits in a Canadian prison population: Prevalence, profile, and outcomes. International journal of law and psychiatry, 44, 7-14. The study noted that 15.4% of the sample had more than two cognitive deficits or at least one severe deficit. Based on the total in-custody male population in 2023-2024 (13,119), the calculation of 3% is derived from the number of enrolments out of the total population of individuals with cognitive deficits (i.e., 60/2,020).
-
Footnote 56
-
“Motivation Module – Support Stream is a time-limited (four sessions), structured intervention for eligible offenders with responsivity factors (literacy, cognitive functioning, etc.) who need additional time and support to understand and apply the skills taught in the program. Through the support stream, program staff work with these offenders to help them complete the program.” – CSC Correctional Programs for Men, accessed from the CSC Hub (March 2025).
-
Footnote 57
-
CSC (November 2020) Evaluation of Correctional Reintegration Programs, Finding 24.
-
Footnote 58
-
CSC (2023). Qualitative examination of specific responsivity factors of correctional program participants with mental health symptoms, cognitive impairment, or learning disabilities. CSC Research Report R-441.
-
Footnote 59
-
Education programs information accessed from the CSC Hub (March 2025)
-
Footnote 60
-
According to CSC, the DEP allows offenders to gain foundational computer skills while upgrading their education and increasing their literacy. Through partnerships with external learning organizations and educational establishments, the DEP provides a blended classroom environment with online learning using an internal digital platform. The platform is tailored to meet the responsivity needs of offenders with various disabilities and learning challenges.
-
Footnote 61
-
Assistive reading and writing technology software and tools.
-
Footnote 62
-
This issue has been raised in several OCI Annual Reports (2019-2020, 2019-2019, 2017-2018, 2011-2012); Woodward, J. (January 2025), Thousands of cellphones are smuggled into Canadian prisons. Advocates are proposing an unusual solution. CTV News. https://www.ctvnews.ca/canada/article/could-supervised-internet-for-inmates-cut-down-on-thousands-of-cellphones-smuggled-into-prison/.
-
Footnote 63
-
FASD Network of Saskatchewan - A community-based, provincial organization with offices in Saskatchewan that works “to enhance the lives of people impacted by FASD”. Through support, training, and events the Network provides services and education across the province. (https://www.saskfasdnetwork.ca/)
-
Footnote 64
-
CSC (2022). Basic needs for safe reintegration: Financial and housing stability (Research in Brief, 21-25).
-
Footnote 65
-
Babchishin, K.M., Keown, L-A., and Mularczyk, K.P. (2021). Economic outcomes of Canadian Federal Offenders. Public Safety Canada and Correctional Service of Canada, Research Report: 2021-R002.
-
Footnote 66
-
Stewart, L. et al. (2017). Reliability and validity of the Dynamic Factors Identification and Analysis – Revised (Research Report R-395). Correctional Service of Canada.
-
Footnote 67
-
Bodkin C., et al. (2019). History of childhood abuse in populations incarcerated in Canada: A systematic review and meta-analysis. American Journal of Public Health.
-
Footnote 68
-
Beaudette, J.N. and Stewart, L.A. (2016). National prevalence of mental disorders among incoming Canadian male offenders. Canadian Journal of Psychiatry; and Brown et al. (2018 April). National prevalence of mental disorders among federally sentenced women offenders: In custody sample (R-406). Correctional Service of Canada.
-
Footnote 69
-
Section 86 of the Corrections and Conditional Release Act.
-
Footnote 70
-
The CCRA makes a distinction between offenders, which is defined as all federally sentenced individuals, and inmates who include only those held in federal penitentiaries.
-
Footnote 71
-
Section 86(2) of the Corrections and Conditional Release Act.
-
Footnote 72
-
CSC (2024 January). Intake, transfer and discharge planning guidelines.
-
Footnote 73
-
See CSC’s Discharge Planning Matrix Tool (August 2023) for discharge planning schedule as well as roles and responsibilities of those involved.
-
Footnote 74
-
CSC. (2012). Mental health strategy for Corrections Canada – A Federal-Provincial-Territorial partnership.
-
Footnote 75
-
OCI. (2004). 2003-2004 Annual Report.
-
Footnote 76
-
CSC. (2008 November). Evaluation report: Community mental health initiative (File #394-2-51). Evaluation Branch, Performance Assurance Sector.
-
Footnote 77
-
Data received on March 24, 2025, through an official documentation request to CSC. Inflation adjusted using the Bank of Canada’s online “Inflation Calculator”, which uses monthly Consumer Price Index data to show changes in the cost of goods. 2007 was used as the base year for comparison, as this was the first year when CMH received full funding.
-
Footnote 78
-
See, Public Safety Canada’s Corrections and Conditional Release Statistical Overview (CCRSO) for federal corrections’ inflation adjusted expenditures.
-
Footnote 79
-
Retrieved on April 10, 2025, from CSC’s Corporate Reporting System – Modernized (CRS-M).
-
Footnote 80
-
For staffing allocation, see Public Safety Canada. (2024). 2022 Corrections and conditional release statistical overview. For CSC’s total planned expenses projected for 2024-2025, see CSC’s 2024-2025 Departmental Plan. Total allocations to Community Corrections in 2024-2025 ($384.5M), inclusive of Community Parole Officers and all expenditures under CSC’s “Community Responsibility Center” were obtained through a data request on June 20, 2025.
-
Footnote 81
-
Email from CSC’s Health Policy and Programs dated December 9, 2024.
-
Footnote 82
-
CSC. (2024 January). Intake, Transfer and Discharge Planning Guidelines.
-
Footnote 83
-
Scale last updated in November 2018. For more info, see CSC’s Mental Health Need Scale – Detailed Instruction Guide.
-
Footnote 84
-
Data received on October 24, 2024, through an official documentation request to CSC.
-
Footnote 85
-
The purpose of Intermediate Mental Health Care (IMHC) is to provide mental health support for incarcerated individuals who have needs that are higher than what can be addressed in primary care, but who do not meet the criteria for care at a Regional Treatment Centre.
-
Footnote 86
-
CSC. (2024 August). Profile of Mental Health Care Patients. Received on December 4, 2024, through an official documentation request to CSC.
-
Footnote 87
-
Beaudette, Power, & Stewart. (2015). National prevalence of mental disorders among incoming federally-sentenced men offenders (Research Report, R-357). Ottawa, ON: Correctional Service Canada.
-
Footnote 88
-
Brown, et al. (2018). Prevalence of mental disorder among federally sentenced women offenders: In-custody and intake samples (Research Report, R-420). Ottawa, ON: Correctional Service Canada.
-
Footnote 89
-
Similarly, the Auditor General’s 2017 report, “Preparing Women Offenders for Release – Correctional Service of Canada” also found that the MHNS did not help mental health staff “prioritize offenders for mental health services.”
-
Footnote 90
-
CSC. (2015 May 4). Discharge Planning: follow-up to Memo “Health Status at Discharge: Gist Report and Matrix Tool” (File number: 276786).
-
Footnote 91
-
For more on CSC’s policies regarding information sharing, see section 19 and 20 of Commissioner’s Directive 800-3: Consent to Health Service Assessment, Treatment, and Release of Information; and sections 11 and 12 of CSC’s “Guidelines for sharing personal health information” (updated March 2018).
-
Footnote 92
-
The OCI understands and respects the professional responsibilities involved in mental health care. However, efforts should be made to clarify how the principles of consent and “need to know” apply in these circumstances.
-
Footnote 93
-
See CSC’s National Essential Health Care Framework (2020 September), where the provision of health services in the community and “essential” health services as per CSC’s obligations under the CCRA, are clarified and defined.
-
Footnote 94
-
CRFs (more commonly known as “halfway houses”) are privately operated, typically by non-profits such as the John Howard Society, Elizabeth Fry Society, St. Leonard’s Society, and the Salvation Army. CCCs are operated by CSC.
-
Footnote 95
-
CSC. (2017 March). Evaluation of Correctional Service of Canada’s health services: Summary. Evaluation Division, Policy Sector. Website.
-
Footnote 96
-
Data received on October 24, 2024, through an official documentation request to CSC.
-
Footnote 97
-
It is important to note that there has been an improvement from 41% with no health card in 2022-23 to 26% in 2023-24. While there has been improvement, this data does not tell us whether the health card was obtained before or during the discharge process, or if it was obtained through the initiative of community staff. Moreover, there are significant regional differences, with 83% having a health card at release in Quebec region in 2023-24, compared 22% in the Pacific Region.
-
Footnote 98
-
For example, see, CSC. (2022). Basic needs for safe reintegration: Financial and housing stability (RIB-21-25).
-
Footnote 99
-
Mental Health Commission of Canada. (2024 February 13). Mental health and the high cost of living: Policy brief.
-
Footnote 100
-
Retrieved from CRS-M module “CCC Population – National Overview” on April 10, 2025.
-
Footnote 101
-
CSC. (2023, January 11). Review of intermediate mental health care services in Correctional Service Canada mainstream institutions and associated recommendations: Overview, purpose, principles and process. Internal Report.
-
Footnote 102
-
Questionnaires were sent to all six maximum-security facilities. However, no response was received from Kent Institution.
-
Footnote 103
-
Based on budget allocation data provided by CSC in April 2025.
-
Footnote 104
-
At the time of writing in January 2025.
-
Footnote 105
-
Based on budget allocation data provided by CSC in April 2025.
-
Footnote 106
-
See the OCI’s 2019-20 Annual Report investigation into Therapeutic Ranges for more on Atlantic Institution's Therapeutic Unit Officer pilot project.
-
Footnote 107
-
The term “women” is used throughout this report, but it is important to note that gender-diverse individuals were also interviewed and included in the investigation.
-
Footnote 108
-
Centre for Addiction and Mental Health (CAMH) https://www.camh.ca/en/health-info/mental-illness-and-addiction-index/trauma
-
Footnote 109
-
Tam, K., & Derkzen, D. (2014). Exposure to trauma among women offenders: A review of the literature (Research Report, R333). Ottawa, ON: Correctional Service of Canada.
-
Footnote 110
-
Ibid.
-
Footnote 111
-
Covington, S. S. (2008). Women and Addiction: A trauma-informed approach. Journal of Psychoactive Drugs, 40(5), 377-385.
-
Footnote 112
-
Malik N., Facer-Irwin E., Dickson H., Bird A., MacManus D. (2023) The Effectiveness of Trauma-Focused Interventions in Prison Settings: A Systematic Review and Meta-Analysis. Trauma Violence Abuse.
-
Footnote 113
-
Felitti, V. J., & Anda, R. F. (2010). The Relationship of Adverse Childhood Experiences to Adult Health, Well-Being, Social Function, and Health care, in R. Lanius, E. Vermetten, & C. Pain (Eds.). The Impact of Early Life Trauma on Health and Disease; The Hidden Epidemic (pp. 77-87). New York: Cambridge University Press.
-
Footnote 114
-
Sheahan, C., & Wardrop, K. (2023). The adverse childhood experiences of Canadian federal offenders: Available information and correctional outcomes (Research Report R-445). Ottawa, Ontario: Correctional Service of Canada.
-
Footnote 115
-
S. Covington. Creating a Trauma-Informed Justice System for Women. The Wiley Handbook on What Works with Girls and Women in Conflict with the Law: A Critical Review of Theory, Practice, and Policy. Edited by L. Gelsthorpe & S. Brown. United Kingdom: John Wiley & Sons Ltd, May 2022.
-
Footnote 116
-
Statistics Canada (2024) Health care access and experiences among Indigenous people, The Daily, November 4, 2024.
-
Footnote 117
-
E.g., Brown, G.P., Barker, J., McMillan, K., Norman, R., Derkzen, D., Stewart, L.A., & Wardrop, K. (2018). Prevalence of mental disorder among federally sentenced women offenders: In-Custody and intake samples (R-420). Ottawa, ON: CSC; Brown, G., Barker, J., McMillan, K., Norman, R., Derkzen, D., & Stewart, L. (2018). National prevalence of mental disorders among federally sentenced women offenders: In custody sample (R-406). Ottawa, ON: CSC; Beaudette, J.N., Power, J., & Stewart, L. A. (2015). National prevalence of mental disorders among incoming federally-sentenced men offenders (R-357). Ottawa, ON: CSC.
-
Footnote 118
-
R-357; R-420.
-
Footnote 119
-
R-420.
-
Footnote 120
-
Source: CSC Data Warehouse – Incidents: Self-inflicted injuries.
-
Footnote 121
-
Schmitt, M. T., Branscombe, N. R., Postmes, T., & Garcia, A. (2014). The consequences of perceived discrimination for psychological well-being: A meta-analytic review. Psychological Bulletin, 140(4), 921–948.
-
Footnote 122
-
E.g., Truth and Reconciliation Commission – Final Report: Honouring the Truth, Reconciling for the Future (2015); House of Commons Standing Committees on Public Safety and National Security (SECU) – Study: Indigenous inmates in the federal correctional system (2017); House of Commons Standing Committee on the Status of Women (FEWO) – Study: Indigenous Women in the Federal Justice and Correctional Systems (2017); National Inquiry into Missing and Murdered Indigenous Women and Girls (NIMMIWG) – Final Report: Reclaiming Power and Place (2020).
-
Footnote 123
-
Taylor, McKendy, & Biro (2023). Understanding the Profile Characteristics and Correctional Experiences of Indigenous Federal Offenders: A Review of Research Results. Correctional Service of Canada: Ottawa ON.
-
Footnote 124
-
Section 84 of the Corrections and Conditional Release Act is part of the release process and applies to individuals who want to serve their conditional or statutory release in an Indigenous community or in an urban area with the support and direction of an Indigenous organization.
-
Footnote 125
-
Backgrounder: United Nations Declaration on the Rights of Indigenous Peoples Act; United Nations Declaration on the Rights of Indigenous Peoples Act (S.C. 2021, c. 14, subsections 1, 2; Article 24).
-
Footnote 126
-
The data reported in these annexes are a snapshot of the OCI’s internal data from the week of April 1, 2025. Future reporting may be different as cases are updated.
-
Footnote 127
-
The number of individuals who contacted our Office to make a complaint (i.e., complainants).
-
Footnote 128
-
Year-end count of in-custody population broken down by regions for fiscal year 2024-25, according to the Correctional Service Canada’s Corporate Reporting System – Modernized (CRS-M).
-
Footnote 129
-
Totals do not include Community Correctional Centres and Community Residential Centres (CCC-CRCs), or Parolees in the community. There were 232 complaints from 159 unique contacts in the community. Also, 242 cases were removed because the complainant(s) wished to remain anonymous.
-
Footnote 130
-
Includes the Special Handling Unit (SHU).
-
Footnote 131
-
Community Correctional Centres and Community Residential Facilities.
-
Footnote 132
-
Totals do not include 242 complaints from anonymous complainants and one case with an unknown facility type.
-
Footnote 133
-
The OCI may commence an investigation on receipt of a complaint by or on behalf of a federally sentenced person, or on its own initiative. Complaints are received by telephone, letters, and during interviews with the OCI's investigative staff at federal correctional facilities.
-
Footnote 134
-
The vast majority of these are general inquiries and administrative calls.
-
Footnote 135
-
Totals do not include 242 complaints from anonymous complainants.
-
Footnote 136
-
An internal resolution involves a response to the complainant through the OCI’s preliminary analysis process. Investigations involve inquiries where steps are taken to determine whether an investigation is warranted, and formal investigations of more complex issues that require analysis as well as dialogue and/or information exchange with multiple sources.
-
Footnote 137
-
A case may be reopened and re-resolved more than once, each with its own reasons for why it is closed. This is the reason that the total in this table is larger than the actual number of complaints reported in Table A.
-
Footnote 138
-
Section 19(1) of the Corrections and Conditional Release Act (CCRA) requires CSC to investigate when “an inmate dies or suffers serious bodily injury” and to “report thereon to the Commissioner or to a person designated by the Commissioner.” As per Section 19(2), CSC is required to provide the OCI with a copy of this report.
-
Footnote 139
-
As per new provisions (adopted in 2019) under Section 19.1(1) of the CCRA, when a CSC healthcare professional advises the Service that there are reasonable grounds to believe a death resulted from natural causes, the Service’s obligations are limited to an internal review of the “Quality of Care” provided to the incarcerated individual.
-
Footnote 140
-
A summary review of CSC’s use of force package is completed for: incidents that are the subject of a specific complaint; where it is determined through triage that the incident requires review; and for level 1 and 2 incidents where CSC’s internal review disputed whether the use of force incident was “necessary” or “proportionate.” A full review is completed for: level 3 incidents; incidents deemed “serious” in nature or occurred in a “location of special interest” to the OCI; incidents where force was used to respond to riots or in circumstances under temporary heightened restrictions; and, incidents where a full Emergency Response Team was deployed.
-
Footnote 141
-
Represents all interactions with federally sentenced individuals, including on the phone, virtually, and in-person.
-
Footnote 142
-
For the purposes of this table, “Interviews” only include those conducted in-person and with federally sentenced individuals. Staff interviews are not included, which is why we are reporting no interviews for some visited facilities. These are instances where all interviews were with staff. Between fiscal years 2020-21 and 2021-22, the Office pivoted to a virtual visit model, which guided how investigators conducted business during the pandemic. These visits involved a combination of videoconferencing and telephone interviews. Readers should keep this in mind when comparing the data in this table to that of previous Annual Reports.
-
Footnote 143
-
Represents the number of days that the OCI spent visiting CSC facilities. Facilities include CSC institutions, CRFs, community parole offices, and other locations where meetings and interviews were conducted with federally sentenced persons.
-
Footnote 144
-
Occasionally, OCI staff conduct visits in teams of two or more. Person Days in Facilities reflects cumulative staff efforts, calculated as the number of days spent on visits to CSC facilities multiplied by the number of individuals on the visiting team (the total captures the number of days on site, per person).
-
Footnote 145
-
Includes Centre régional de santé mentale.
-
Footnote 146
-
Includes the Regional Treatment Centre – Bath.
-
Footnote 147
-
Includes Joyceville’s Assessment Unit and Temporary Detention Unit.
-
Footnote 148
-
Includes the Regional Treatment Centre - Millhaven, Assessment Unit, and the Temporary Detention Unit.
-
Footnote 149
-
In 107 cases, the complainants requested to remain anonymous. One concerned a provincial matter outside of the OCI’s jurisdiction.